Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 | |
 |  |
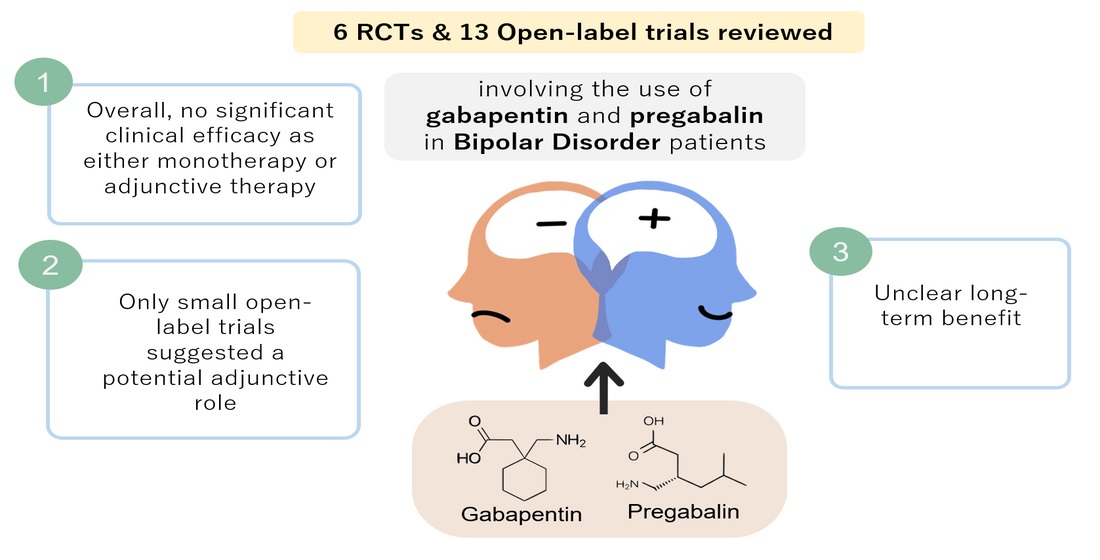
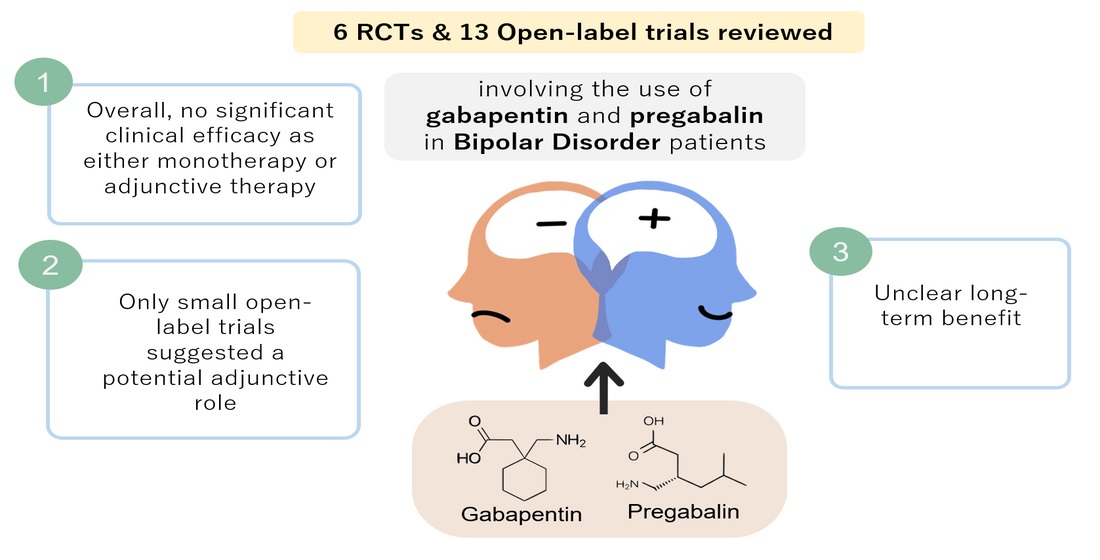
 |  |
Although failing to show clear antimanic efficacy in randomized trials, gabapentin still remains a clinically useful agent when it comes to combination treatment in refractory and co-morbid patients. Results: Gabapentin was moderately to mark-edly effective in 30% (15/50) of patients, with statistically nonsignificant differences between patients with bipolar disorder type I, bipolar dis-order type II and NOS, and unipolar major de-pressive disorder. 70% reported side effects, mainly sedation, with 16% of the total sample discontinuing treatment due to adverse events. Conclusion Gabapentin is a nerve pain medication and anticonvulsant that has proven to be effective for people who have hard-to-treat depression or other mood disorders. Subject terms: Neuroscience, Bipolar disorder Introduction The gabapentinoids comprise gabapentin and pregabalin. Gabapentin is licensed for use in the USA for the treatment of focal seizures and post-herpetic neuralgia [1] and in the UK for focal seizures and peripheral neuropathic pain [2]. Two new anticonvulsants, lamotrigine and gabapentin, have been used increasingly for bipolar disorder in the past several years. Despite this array of options, bipolar disorder remains a difficult disorder to treat. Some subtypes, such as those characterized by rapid cycling or mixed episodes, have been especially resistant to lithium treatment. Gabapentin may help with some symptoms of bipolar disorder, but there’s limited evidence supporting its effectiveness, and it’s not FDA approved for bipolar. Gabapentin may be a useful drug for the add-on treatment of bipolar patients with poor response to other mood stabilizers. Gabapentin may improve depressive residual symptoms such as irritability, social withdrawal or anxiety. These results should be confirmed in randomized clinical trials. Explore gabapentin's role in mental health treatment, including its uses, benefits, and potential risks. Learn about dosage, effectiveness, and side effects. The use of gabapentin in bipolar disorder (BPD) treatment provides an informative case of off-label uptake and abandonment of a new medication. Gabapentin was patented by Warner-Lambert in 1977 and FDA-approved in December1993 for the adjunctive treatment of epilepsy and in 2002 for postherpetic neuralgia (see Appendix 1 for timeline). A systematic search strategy employing different combinations of the keywords (bipolar, mania, hypomania, gabapentin, neurontin, gralise, gabarone, fanatrex, pregabalin, lyrica) was developed and performed in five databases namely OVID Medline, PubMed, ProQuest, PsychInfo and ScienceDirect from database inception to 7 June 2021. Key takeaways: Gabapentin is a medication that’s used to treat seizures, nerve pain from shingles, and restless leg syndrome. Despite previous marketing claims, there’s no evidence that gabapentin is a good treatment for bipolar disorder. The best treatment for bipolar disorder is therapy and a combination of other medications. These include mood stabilizers, anticonvulsants, and Introduction Gabapentin has been extensively prescribed off-label for psychiatric indications, with little established evidence of efficacy. Gabapentin and pregabalin, a very similar drug with the same mechanism of action, bind to a subunit of voltage-dependent calcium channels which are implicated in the aetiopathogenesis of bipolar disorder, anxiety and insomnia. This systematic review and Abstract Background: Gabapentin, a new anti-epileptic agent, has been anecdotally reported to be effective in the treatment of mania. We systematically assessed the response rate in bipolar patients being treated adjunctively with gabapentin for manic symptoms, depressive symptoms, or rapid cycling not responsive to standard treatments. This article reviews evidence-based psychiatric uses of gabapentin, along with associated risks. An extensive literature review was conducted, primarily of articles searchable in PubMed, relating to psychiatric uses, safety, and adverse effects of The gabapentinoids, gabapentin, and pregabalin, target the α<sub>2</sub>δ subunits of voltage-gated calcium channels. Initially licensed for pain and seizures, they have become widely prescribed drugs. Many of these uses are off-label for psychiatric indications, and there is increasing concern abou Gabapentin is commonly used off-label in the treatment of psychiatric disorders with success, failure, and controversy. A systematic review of the literature was performed to elucidate the evidence for clinical benefit of gabapentin in psychiatric with bipolar I, bipolar II, and treat-ment-resistant depression.3 Thus, the new FDA approvals for bipolar mania for quetiapine and ziprasidone and pending for aripiprazole mean the possibility of adding new options to the treatment formula for bipolar spectrum disorders, including some with less risk of weight gain and per-haps diabetes.10 Any For bipolar disorder, four double-blind RCTs investigating gabapentin, and no double-blind RCTs investigating pregabalin, were identified. Unfortunately, gabapentin does not demonstrate efficacy in randomized trials for bipolar disorder and current treatment guidelines do not emphasize its use. Despite of the lack of evidence, reviews of gabapentin prescribing patterns in the United States show that this medication is still being used with alarming frequency for bipolar disorder.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 | |
 |  |
 |  |