Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
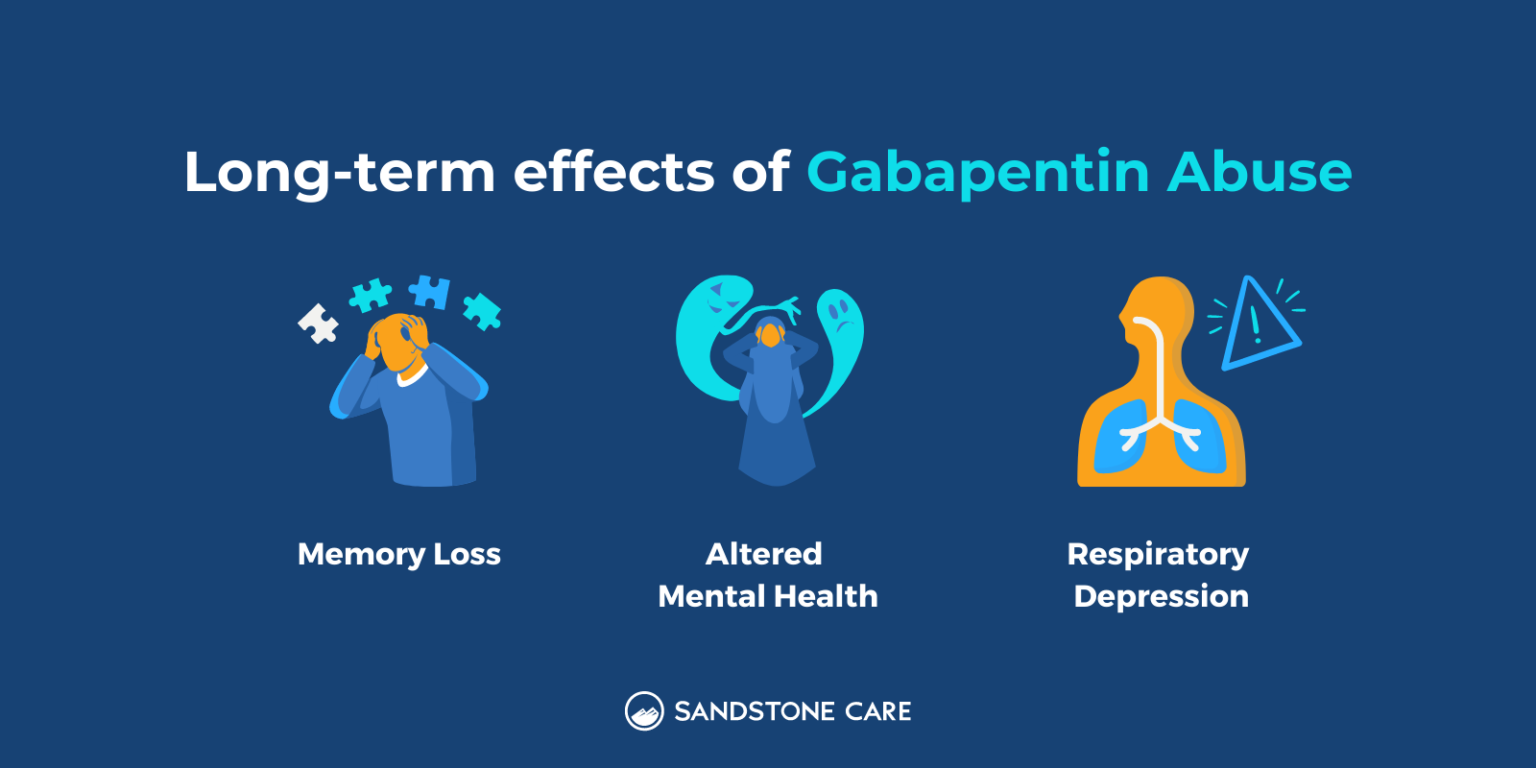
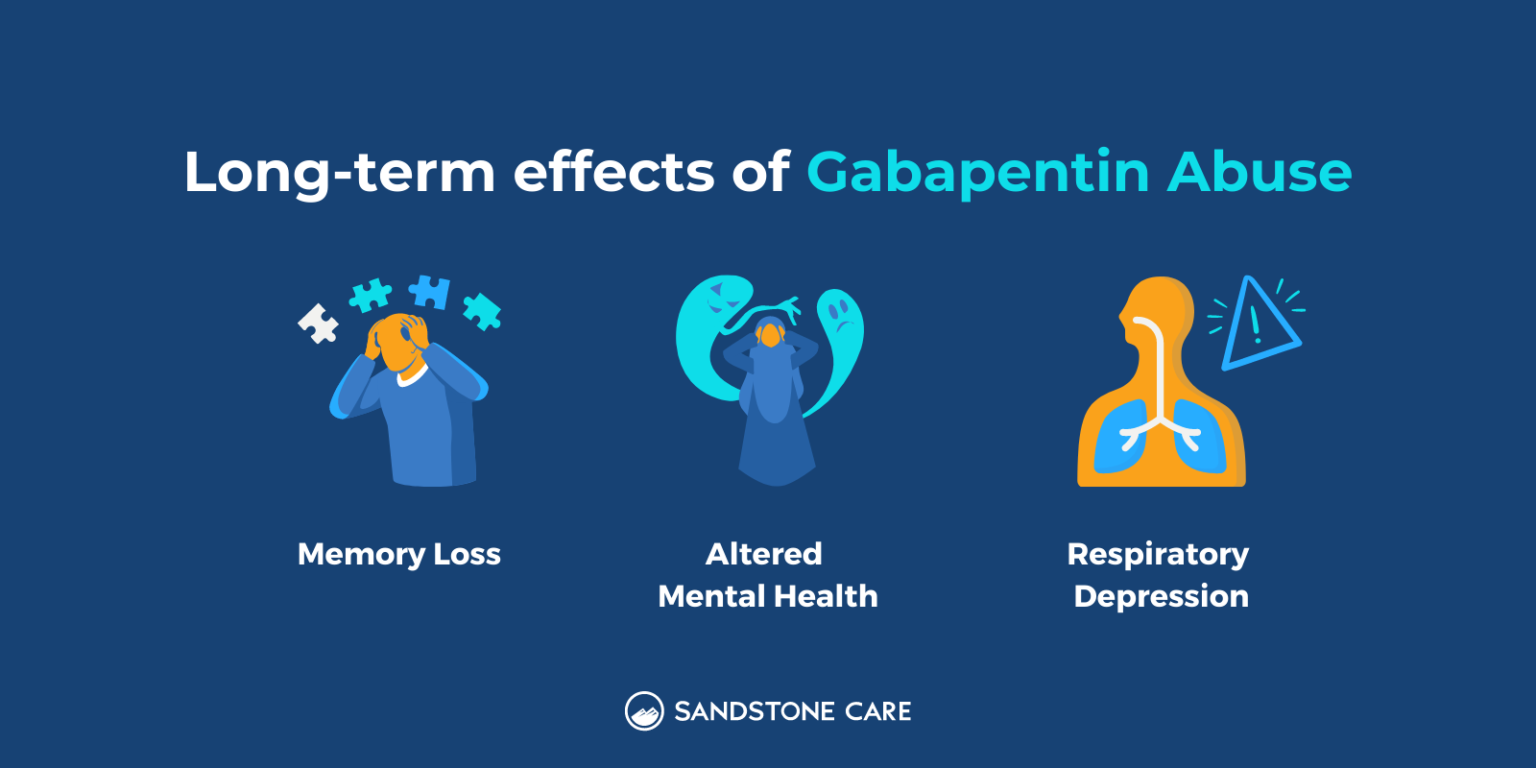
In conclusion, clinicians should be aware of reversible causes of acute dysphagia including jaw myoclonus. Gabapentin could be a cause of drug-induced jaw myoclonus. Myoclonus is a well-reported complication of gabapentin toxicity especially in patients with renal impairment. As gabapentin is solely excreted by the kidneys, renal dose adjustment is recommended in the literature. Gabapentin and pregabalin toxicity can manifest as myoclonus. While myoclonus can present in multiple ways – focal or multifocal, positive, negative, and rest, cortical or subcortical – it most often occurs in a positive or rest, multifocal, and subcortical fashion. Pregabalin- and gabapentin-induced negative myoclonus can develop even in patients with normal renal function. Physicians should keep in mind the possibility of patients developing negative myoclonus under treatment of pregabalin or gabapentin even in short period of time and with low dosage, and in the normal range of renal function. GBP-associated myoclonus appears to be relatively frequent. It is usually mild and can easily be overlooked. Discontinuation of therapy is not necessary in most cases. Discussion While there are several prior case reports of gabapentin-induced myoclonus, facial myoclonus does not appear to have been documented in the literature. Specifically, there is a lack of literature in emergency medicine regarding gabapentin-induced myoclonus. The underlying cause of this pathology has yet to be fully elucidated. Abstract Gabapentin (GBP) and pregabalin (PGB) are FDA approved for adjunctive treatment of partial seizures and for treatment of post-herpetic neuralgia. Both drugs are primarily eliminated by renal excretion. However, PGB or GBP induced myoclonus has only been reported infrequently in case reports/series. It is not discussed with patients and its sudden occurrence can lead to anxiety because Background: Myoclonus may be linked to a variety of causes, including epilepsy, postanoxic brain injury, metabolic encephalopathies and focal central nervous system lesions. Various drugs also have been reported to induce myoclonus. Gabapentin-induced myoclonus has been reported previously, especially in cases with impaired renal function or epilepsy. Pregabalin- and gabapentin-induced negative myoclonus can develop even in patients with normal renal function. Physicians should keep in mind the possibility of patients developing negative myoclonus under treatment of pregabalin or gabapentin even in short period of time and with low dosage, and in the normal range of renal function. Further prospective study investigating incidence and risk Gabapentin and pregabalin toxicity can manifest as myoclonus. While myoclonus can present in multiple ways – focal or multifocal, positive, negative, and rest, cortical or subcortical – it most often occurs in a positive or rest, multifocal, and subcortical fashion. Gabapentin (GBP) and pregabalin (PGB) are FDA approved for adjunctive treatment of partial seizures and for treatment of post-herpetic neuralgia. Both drugs are primarily eliminated by renal excretion. However, PGB or GBP induced myoclonus has only been reported infrequently in case reports/series. It is not discussed with patients and its sudden occurrence can lead to anxiety because of With regard to positive myoclonus, it has been suggested that the serotonin neurotransmitter system plays a role in the development of gabapentin-induced myoclonus [10 - 12]. PGB and gabapentin have a similar chemical structure and show the same mechanism of action. Gabapentin is the first-line treatment for painful diabetic polyneuropathy. [2] Gabapentin is primarily excreted from the kidneys and the clearance of gabapentin is altered in patients with deranged renal function. [3] Gabapentin toxicity can be manifested with symptoms such as myoclonus, [4] hypoglycemia, [5] and altered sensorium. [6] Prior to admission, the patient had been chronically treated with gabapentin 900 mg total daily dose for neuropathic pain. With discontinuation of gabapentin and initiation of HD, marked improvement in her myoclonus occurred. In conclusion, clinicians should be aware of reversible causes of acute dysphagia including jaw myoclonus. Gabapentin could be a cause of drug-induced jaw myoclonus. Negative myoclonus is a jerky, brief, and sudden interruption of voluntary muscle contraction. Although gabapentin and pregabalin have been reported to induce positive myoclonus in some patients with impaired renal function, there are only a few studies describing pregabalin- or gabapentin-induced negative myoclonus. Acute hyperkinetic movement disorders such as multifocal or segmental myoclonus in elderly patients warrant a prompt review of recent drug history, especially gabapentin, even in the background of normal renal function. The type of myoclonus is dependent on the comorbidity, either renal dysfunction or epilepsy, and should be managed accordingly. With a high index of suspicion, aggressive testing and treatment for other possible conditions like seizures (in non-epilepsy patients) or CNS infections can be avoided. Abstract Introduction: Negative myoclonus is a jerky, brief, and sudden interruption of voluntary muscle contraction. Although gabapentin and pregabalin have been reported to induce positive myoclonus in some patients with impaired renal function, there are only a few studies describing pregabalin- or gabapentin-induced negative myoclonus. This study reviewed patients who had developed Myoclonus is a rare side effect of gabapentin (GBP) and has been reported in patients with preexisting myoclonus, mental retardation, chronic static encephalopathy, diffuse brain damage, impaired renal function, or end stage renal disease. We report
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |