Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
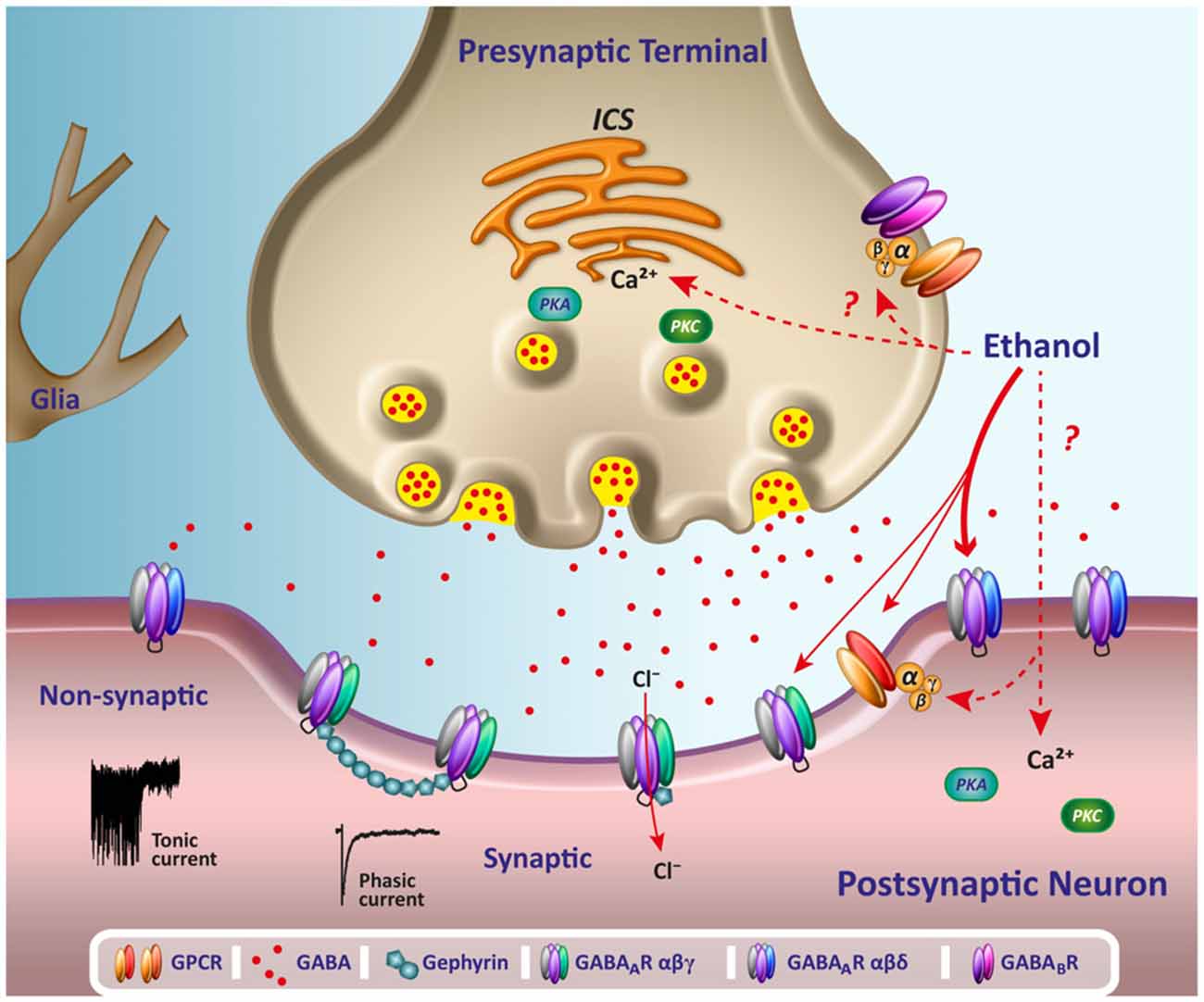
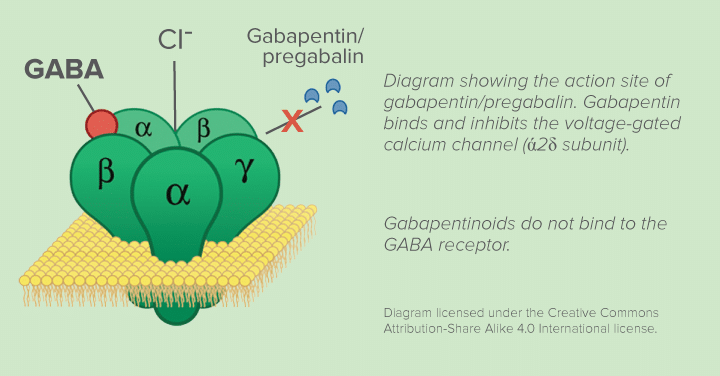
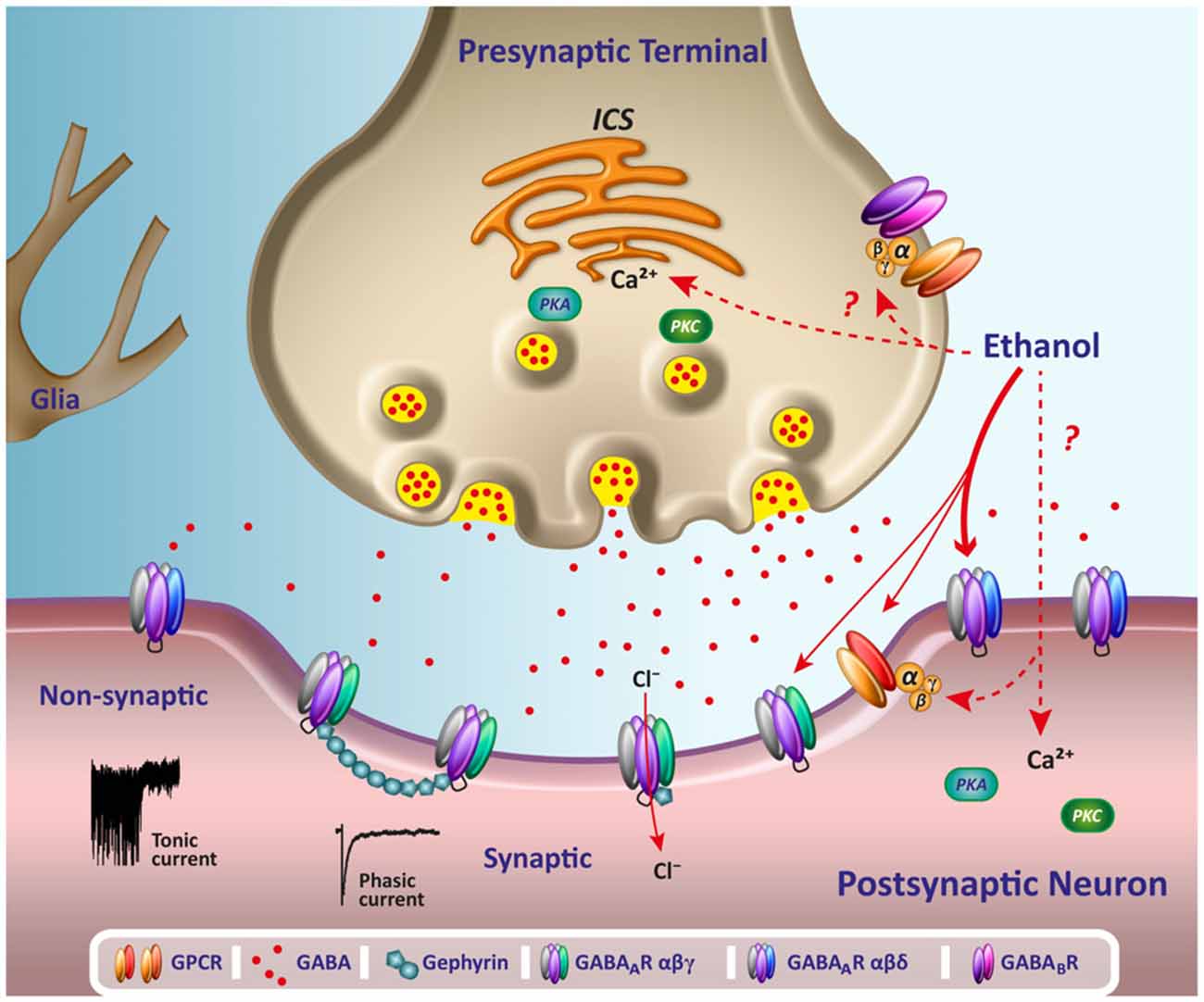
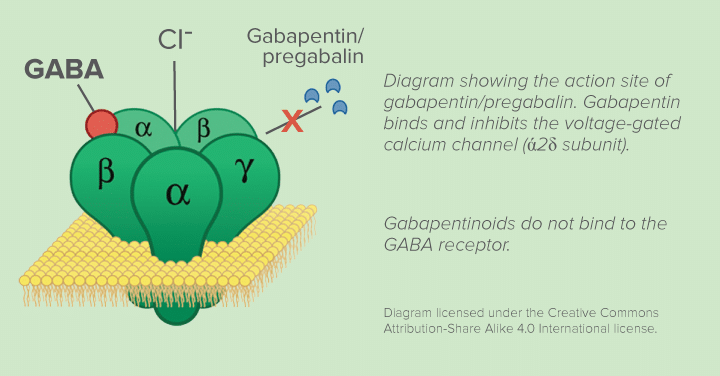
A comprehensive list of conditions and drugs that may prolong the QT interval, and cause torsade de pointes (TdP) and long QT syndrome (LQTS) is presented below. With regards to drugs, the risk of QT prolongation and TdP varies markedly across the list but tends to be rather similar within a drug class. While the risk of TdP is well-defined for many of these agents, many are classified as QT Pratt CM, Ruberg S, Morganroth J, et al. Dose-response relation between terfena-dine (Seldane) and the QTc interval on the scalar electrocardiogram: distinguishing a drug effect from spontaneous Objective: As part of the overall safety evaluation of gabapentin enacarbil, the present definitive QT/QTc study was conducted to assess the effects of gabapentin enacarbil on cardiac repolarization in accordance with the International Conference on Harmonization E14 guidance. An article from the neurology section of GPnotebook: Drugs causing QT prolongation. Many drug therapies are associated with prolongation of the QT interval. This may increase the risk of Torsades de Pointes (TdP), a potentially life-threatening cardiac arrhythmia. As the QT interval varies with a change in heart rate, various formulae can adjust for this, producing a 'corrected QT' Objective As part of the overall safety evaluation of gabapentin enacarbil, the present definitive QT/QTc study was conducted to assess the effects of gabapentin enacarbil on cardiac repolarization in accordance with the International Conference on Harmonization E14 guidance. Mood stabilizers Among the mood stabilizers, lithium [22] has a moderate risk of QTc prolongation while the antiepileptics used for this purpose such as carbamazepine, oxcarbazepine, topiramate, valproate, [26] pregabalin, gabapentin, [27] and lamotrigine [28] are reported to be safe with a low risk of QTc prolongation. Table 1 summarises normal, borderline, prolonged and sub-stantially elevated risk QTc measurements in males and females. If a patient presents with a prolonged QTc interval, then modifiable risk factors should be investigated and addressed, eg electrolyte disturbances. Where possible, an alternative drug that does not have an effect on the QT interval may also be considered. Prescribers should Table 1 summarises normal, borderline, prolonged and substantially elevated risk QTc measurements in males and females. If a patient presents with a prolonged QTc interval, then modifiable risk factors should be investigated and addressed, eg electrolyte disturbances. Where possible, an alternative drug that does not have an effect on the QT interval may also be considered. Prescribers should For esomeprazole, no effect on ECG parameters could be found in healthy volunteers 1.5 or 3 hours after a 40 mg dose [67]. In another case report, addition of lansoprazole in a patient already taking disopyramide, a class Ia antiarrhythmic agent, was associated with development of in long QT syndrome (QTc 690 ms) and TdP [68]. Data about the effect of Propofol on QTc is conflicting, while we certainly know that this drug does not modify TDR [55 - 58]. Moreover, Propofol rapidly reverses Sevoflurane-induced QTc prolongation in healthy patients and therefore may be beneficial [59]. My GP does not know what to prescribe but has suggested fluoxetine or sertraline both of which are on the drugs to avoid list. My chronic back pain clinic consultant has also been unable to suggest a medication for fibromyalgia and has only given me lidocaine patches which do not appear to work at all. Any suggestions? The heart has an electrical system that allows it to contract in a rhythm. A vital aspect of this electrical system is depolarization and repolarization. The focus of this activity is on the QT interval. It is measured from the Q wave until the T wave, and the QT interval clinically represents the repolarization of the ventricles. Many commonly used medications exhibit QT-prolonging effects Purpose of Review The objective of this manuscript is to describe the cardiovascular effects of the gabapentinoids gabapentin and pregabalin. Recent Findings The most frequent adverse effects of gabapentin and pregabalin affect the central nervous system, such as somnolence and fatigue. Additionally, pregabalin, and a much lesser extent, gabapentin, may adversely affect the cardiovascular Among the mood stabilizers, lithium [22] has a moderate risk of QTc prolongation while the antiepileptics used for this purpose such as carbamazepine, oxcarbazepine, topiramate, valproate, [26] pregabalin, gabapentin, [27] and lamotrigine [28] are reported to be safe with a low risk of QTc prolongation. This guideline standardizes the requirements necessary when studying QT/QTc interval prolongation and proarrhythmic potential of non-antiarrhythmic drugs. According to E14, a negative study is one in which the upper bound of the 1-sided 95% confidence interval of the maximum change in QTc interval for a drug is less than 10 ms. Summary: Long qt syndrome is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are female, 60+ old, also take Aspirin, and have High blood pressure. The phase IV clinical study analyzes which people have Long qt syndrome when taking Gabapentin. Female gender has been documented in many studies as a risk factor, with females having baseline QTc intervals that are generally 20 milliseconds greater than that of males. 2,3 Cardiac conditions such as bradycardia and heart failure have also been indicated as nonpharmacologic risk factors for drug-induced QT prolongation and TdP. The BNF 86 (September 2023 – March 2024) also lists the following drugs that are predicted by the manufacturer to increase the risk of QT prolongation, and therefore concurrent use alongside drugs that prolong the QT interval should be avoided: Drugs associated with QT Prolongation, QTc prolongation including Antipsychotics, antiarrhythmics, antidepressants, and antihistamines
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |