Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 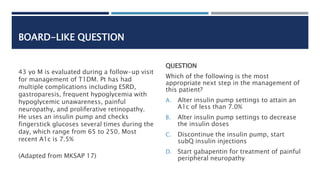 |
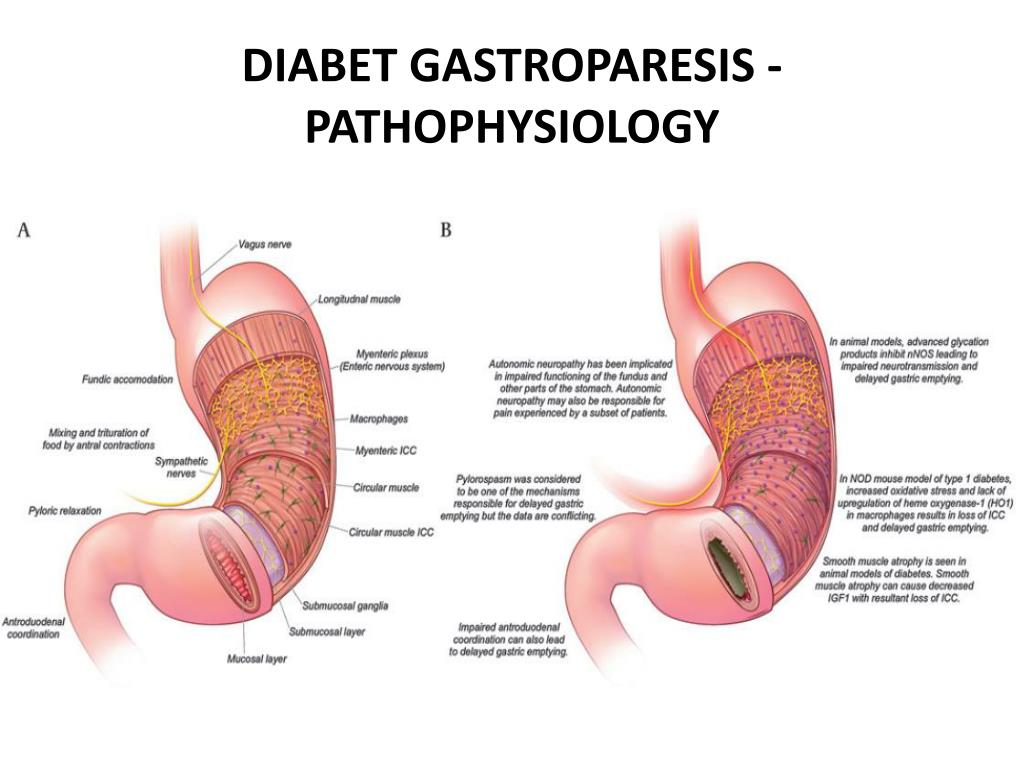
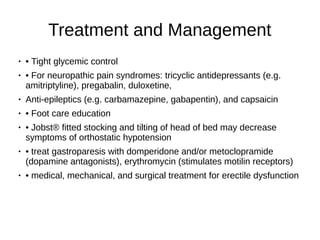
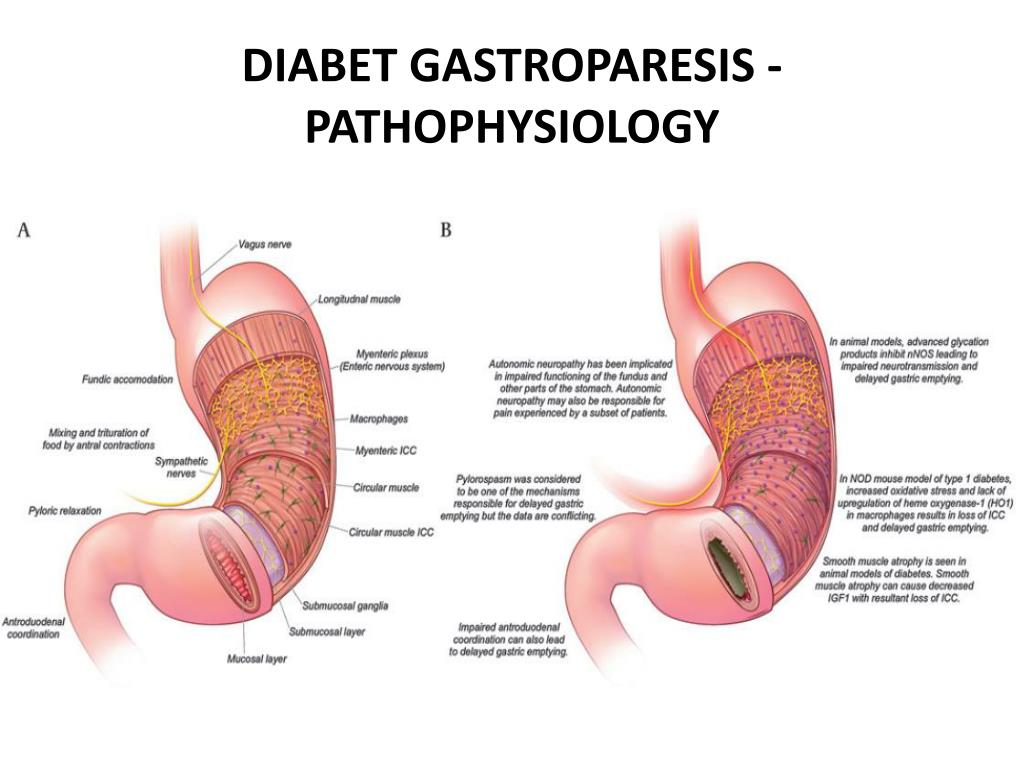
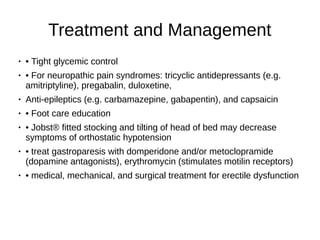
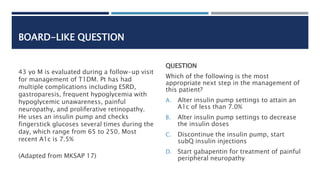
Gabapentin and Diabetic gastroparesis - a phase IV clinical study of FDA data Summary: Diabetic gastroparesis is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are female, 60+ old, also take Lantus, and have Gastroesophageal reflux disease. INTRODUCTION Gastroparesis is a syndrome of objectively delayed gastric emptying in the absence of a mechanical obstruction and cardinal symptoms of nausea, vomiting, early satiety, belching, bloating, and/or upper abdominal pain. This topic will review the treatment of gastroparesis. The pathophysiology, etiology, and diagnosis of gastroparesis are discussed separately. (See "Pathogenesis of Gastroparesis (GP), a historically vexing disorder characterized by symptoms of nausea, vomiting, abdominal pain, early satiety, and/or bloating, in the setting of an objective delay in gastric emptying, is often difficult to treat and carries a Currently, some doctors are prescribing the gabapentin to prevent migraine headaches, treat nystagmus, and reduce neuropathic pain. [5, 6, 7] However, there are few studies on analgesic effects of gabapentin and other effects of it. I have gastroparesis and taking Gabapentin how long does it take to get used to symptoms especially fatigue? Do you eventually adjust? Gastroparesis is defined by delayed gastric emptying and symptoms of nausea, vomiting, bloating, postprandial fullness, early satiety and abdominal pain. Most common etiologies include diabetes, post-surgical and post-infectious, but in most cases It is structurally related to gabapentin but has no activity at GABA or benzodiazepine receptors, though both pregabalin and gabapentin are frequently used to treat neuropathic pain. Gabapentin is a medication primarily used for nerve pain and seizures, but it's often used off-label for gastroparesis. It's thought to help regulate nerve signals in the digestive system, potentially improving stomach emptying. If possible, however, try to use Gabapentin, Pregablin or tricyclics such as Nortriptyline for the abdominal pain in gastroparesis. There are patients who are refractory to all types of treatment and cannot even take in sufficient calories and fluids. This guideline presents recommendations for the evaluation and management of patients with gastroparesis. Gastroparesis is identified in clinical practice through the recognition of the clinical symptoms and documentation of delayed gastric emptying. Symptoms from gastroparesis include nausea, vomiting, early satiety, postprandial fullness, bloating, and upper abdominal pain. Management of Key findings This retrospective, open-label study evaluated the efficacy of low-dose gabapentin in 62 adults with functional dyspepsia and normal gastric emptying Gabapentin resulted in significant improvements in dyspeptic symptoms as measured by change in total score and most subscale scores on the Patient Assessment of Gastrointestinal Disorders–Symptom Severity Index (PAGI-SYM) The Delayed gastric emptying on objective testing defines gastroparesis, but symptoms overlap with functional dyspepsia and do not correlate well with gastric emptying delay. This review outlines a strategy for defining, diagnosing, and managing refractory gastroparesis. This case report discusses 2 cases of medication-induced gastroparesis which were initially diagnosed as diabetic gastroparesis, and thorough history taking revealed the cause to be medication induced. Repeat studies following medication discontinuation revealed improvement in symptoms and resolution of gastroparesis. An accurate diagnosis is necessary to treating gastroparesis, since the treatment depends on the cause. If your doctor diagnosed an underlying disease or condition that is causing the gastroparesis, the treatment will focus on correcting or reversing that condition; if there is no underlying cause Discussion This case underscores the complexity of managing severe feeding intolerance in infants, particularly with concomitant conditions like visceral hyperalgesia and gastroparesis. Despite multiple interventions, including ND tube placement and TPN, the patient experienced persistent feeding intolerance. The introduction of gabapentin, informed by emerging evidence and its application in Abstract Gastroparesis is a gastrointestinal motility disorder characterized by nausea, vomiting, early satiation, postprandial fullness, bloating, and upper abdominal pain. The diagnosis requires documented delay in gastric emptying with an optimal test such as scintigraphy or stable isotope gastric emptying breath test in the absence of mechanical obstruction. The pathophysiologic mechanisms In this case, we highlight the utility of a gabapentin trial in an otherwise healthy patient. This case underscores the complexities of managing severe feeding disorders in infants, particularly the role of gabapentin in addressing suspected visceral hyperalgesia and failure to thrive in a patient without previous neurological or cardiac surgery. This guideline presents recommendations for the evaluation and management of patients with gastroparesis. Gastroparesis is identified in clinical practice through the recognition of the clinical symptoms and documentation of delayed gastric New to gastroparesis? Please view our megathread for a detailed explanation of gastroparesis as well as the main medicines and procedures used to manage symptoms, as well as list of popular neurogastroenterologists and motility clinics. Join these gastroparesis support groups (Discord, Facebook, etc.) today using this link. Treatment Treating gastroparesis begins with finding and treating the condition that's causing it. If diabetes is causing your gastroparesis, your healthcare professional can work with you to help you control your blood sugar levels.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |