Gallery
Photos from events, contest for the best costume, videos from master classes.
/VWH_Illustration_At-Home-Treatment-for-Knee-Pain_Illustrator_Laura-Porter_No-Text_Final-17e5c794f85f43cba3c260f621c34298.gif) |  |
/x-ray-illustration-of-hip-replacement-1254389825-b985fdb1364345f1892cde5cd397eee5.jpg) | 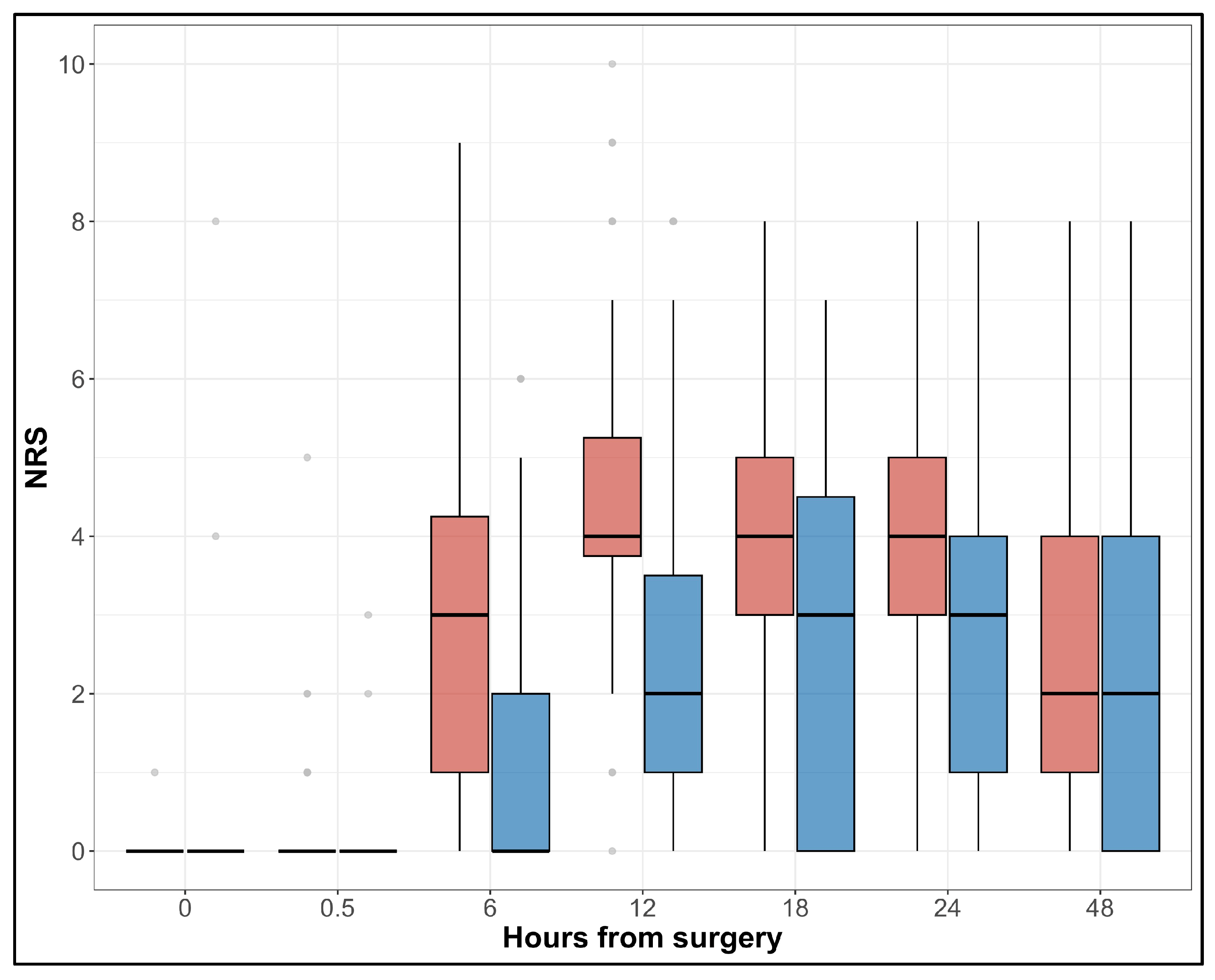 |
 |  |
 |  |
 |  |
/Verywell-25-2696611-SingleLegBridge01-1814-59934340396e5a0010a7c3d5.gif) |  |
Background Postoperative pain after total knee arthroplasty (TKA) and total hip arthroplasty (THA) influence patients’ rehabilitation and life quality. Although gabapentin has been widely used for analgesia, its efficacy is still controversial in TKA and THA. This meta-analysis was performed to assess the efficacy and safety of gabapentin following TKA and THA. Method Electronic databases The efficacy of perioperative gabapentin for the treatment of postoperative pain following total knee and hip arthroplasty: a meta-analysis We did not identify statistically significant or clinically meaningful differences in our primary and secondary outcomes related to perioperative use of gabapentin enacarbil in patients having primary hip or knee arthroplasties. Abstract Background: Pain management after total hip arthroplasty (THA) varies and has been widely studied in recent years. Gabapentin as a third-generation antiepileptic drug that selectively affects the nociceptive process has been used for pain relief after THA. This meta-analysis was conducted to examine the efficacy of gabapentin in THA. Surgeons have made substantial efforts to decrease postoperative opioid prescribing, largely because it can lead to prolonged use. These efforts include adoption of non-opioid pain medication including gabapentin. Like opioids, gabapentin use may be US Pharm. 2011;36 (11):Epub. Each year, hip fractures contribute to more than 225,000 hospitalizations in Medicare recipients, and this number is expected to double by the year 2040. 1 Length of stay for total hip arthroplasty (THA) has declined from 1991 to 2008, but this has resulted in an increase in post–acute care admissions and rehospitalizations. 2 According to the National Center for The following medical subject heading terms, keywords, and their combinations were used: “pain management, postoperative pain, total hip arthroplasties, total hip replacement, and gabapentin”. The search was limited to randomised controlled trials (RCTs) in humans and published in English up to December 2015. M, et al. Perioperative gabapentin reduces 24 h opioid consumption and improves in-hospital rehabilitation but not post-discharge outcomes after total knee arthroplasty with peripheral nerve block. Bja Br J Anaes Neuroactive Medications Another type of medicine used as part of a multimodal pain regimen after hip replacement are medicines that target nerve pain – namely gabapentin (Neurontin) or pregabalin (Lyrica). Using these medications decreases the amount of opioids required after hip replacement. Background: Postoperative pain after total knee arthroplasty (TKA) and total hip arthroplasty (THA) influence patients' rehabilitation and life quality. Although gabapentin has been widely used for analgesia, its efficacy is still controversial in TKA and THA. This meta-analysis was performed to assess the efficacy and safety of gabapentin following TKA and THA. Method: Electronic databases Should I Stop Taking Gabapentin Before Hip Replacement Surgery? Gabapentin can lead to sedation and enhance the effects of certain pain medications, such as opioids, used before or after surgery. Adjusting medication doses may be necessary to prevent issues if surgery is scheduled. Informing doctors about all medications before surgery is crucial. Learn about the use of gabapentin as a potential treatment option after hip replacement surgery and its effectiveness in managing pain and improving recovery. The following medical subject heading terms, keywords, and their combinations were used: “pain management, postoperative pain, total hip arthroplasties, total hip replacement, and gabapentin”. The search was limited to randomised controlled trials (RCTs) in humans and published in English up to December 2015. Gabapentin is routinely used in preoperative multimodal anesthesia to reduce pain following total joint arthroplasty (TJA) surgery. Evolving evidence has shown it is ineffective in reducing postoperative pain and should be used cautiously in this patient population due to its adverse effects. The pu Gabapentin is routinely used in preoperative multimodal anesthesia to reduce pain following total joint arthroplasty (TJA) surgery. Evolving evidence has shown it is ineffective The American Association of Hip and Knee Surgeons, The American Academy of Orthopaedic Surgeons (AAOS), The Hip Society, The Knee Society, and The American Society of Regional Anesthesia and Pain Medicine have worked together to develop evidence-based guidelines on the use of gabapentinoids in primary total joint arthroplasty (TJA). The purpose of these guidelines is to improve the treatment Background Multimodal analgesia regimens are recommended for the postoperative period after hip and knee replacement surgeries. However, there are no data on practice patterns for analgesic use in the immediate postoperative period after hip and knee replacements in Australia. Objectives To describe analgesic prescribing patterns in the inpatient postoperative phase for patients undergoing hip The following keywords including pain management, postoperative pain, total knee arthroplasties, total knee replacement, and gabapentin were used for searching. Gabapentin, a drug traditionally used for the relief of neuropathic pain, was compared in variable doses to placebo in relieving postoperative pain. Gabapentin resulted in less total patient-controlled analgesia (PCA) morphine use over 48 hours postoperatively (P <0.05), better active knee flexion on postoperative days (PODs) 2 and 3 (P <0.05 for both), and less pruritus (P <0.05) than placebo Jeanette R. Schultz Gabapentin is routinely used in preoperative multimodal anesthesia to reduce pain following total joint arthroplasty (TJA) surgery. Evolving evidence has shown it is ineffective in reducing postoperative pain and should be used cautiously in this patient population due to its adverse effects. The purpose of this work was to implement an evidence-based practice (EBP) change
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
/VWH_Illustration_At-Home-Treatment-for-Knee-Pain_Illustrator_Laura-Porter_No-Text_Final-17e5c794f85f43cba3c260f621c34298.gif) |  |
/x-ray-illustration-of-hip-replacement-1254389825-b985fdb1364345f1892cde5cd397eee5.jpg) | 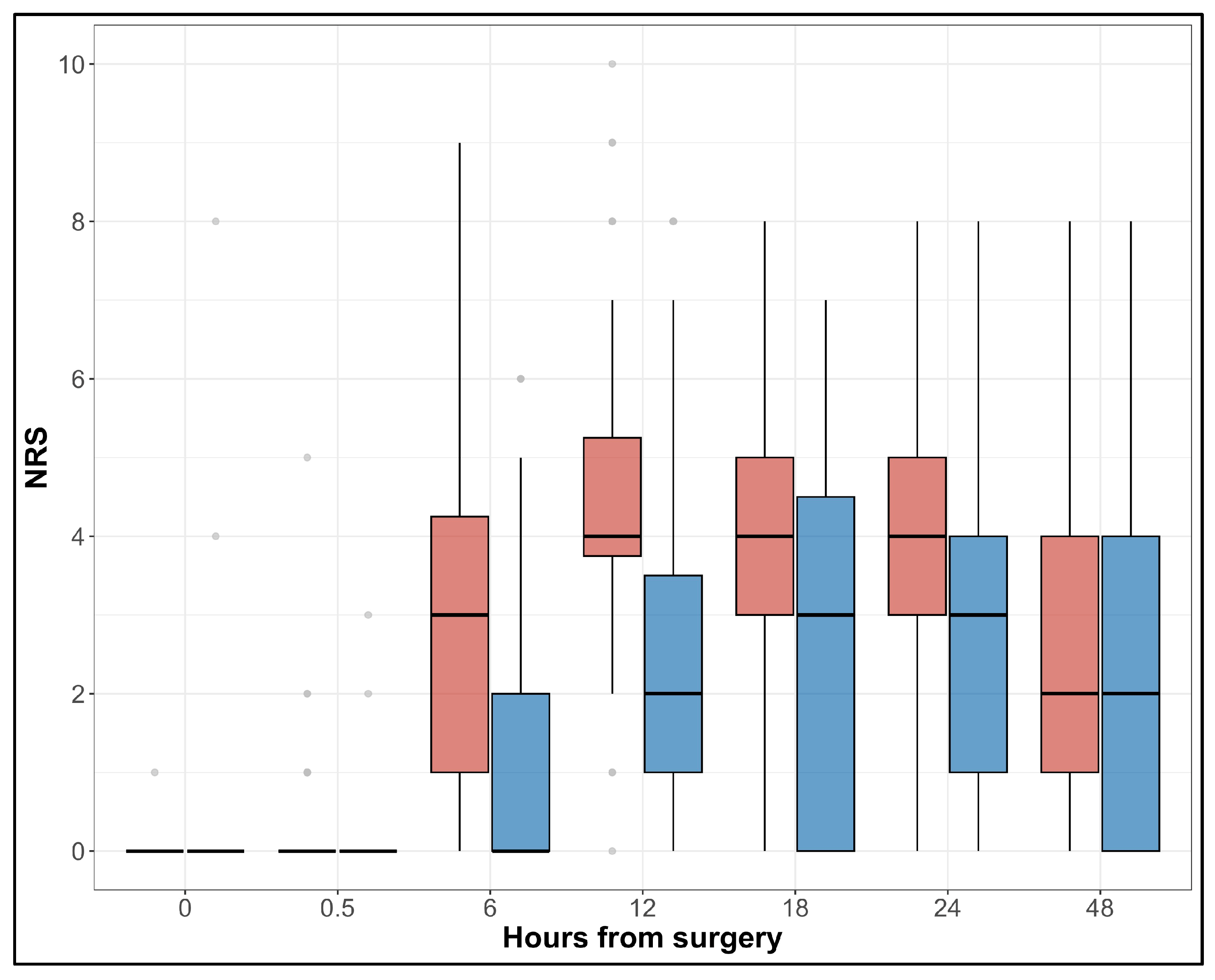 |
 |  |
 |  |
 |  |
/Verywell-25-2696611-SingleLegBridge01-1814-59934340396e5a0010a7c3d5.gif) |  |