Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | |
 | 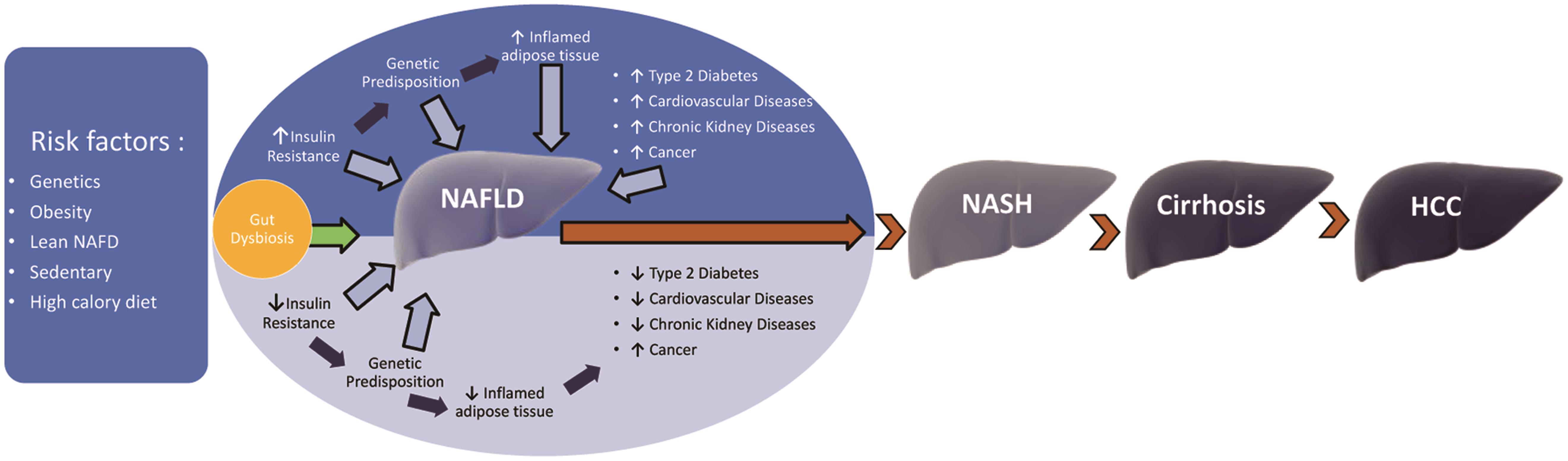 |
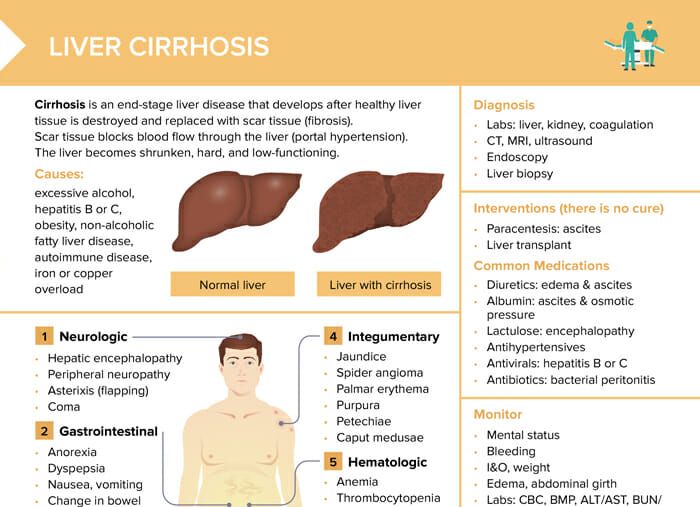
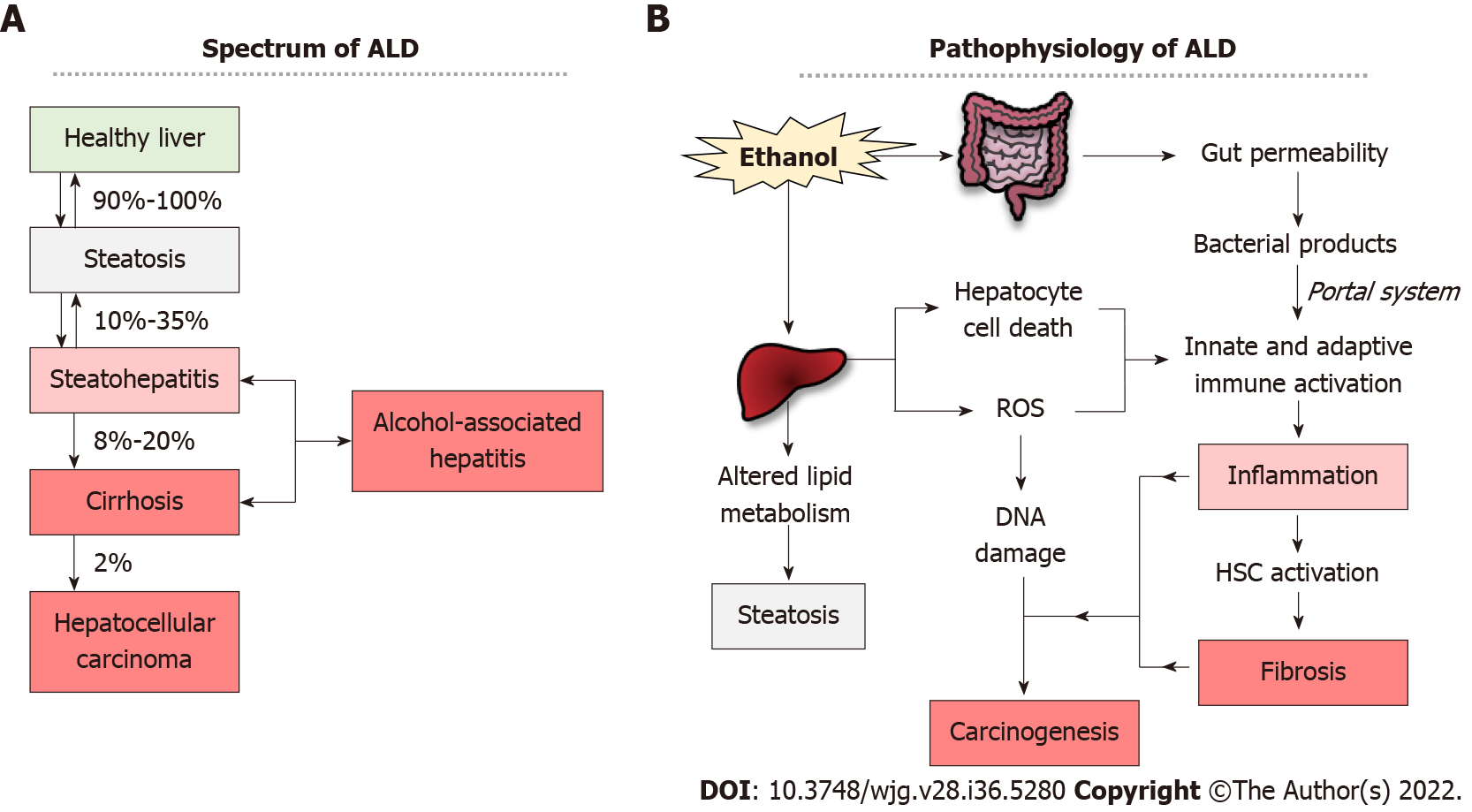
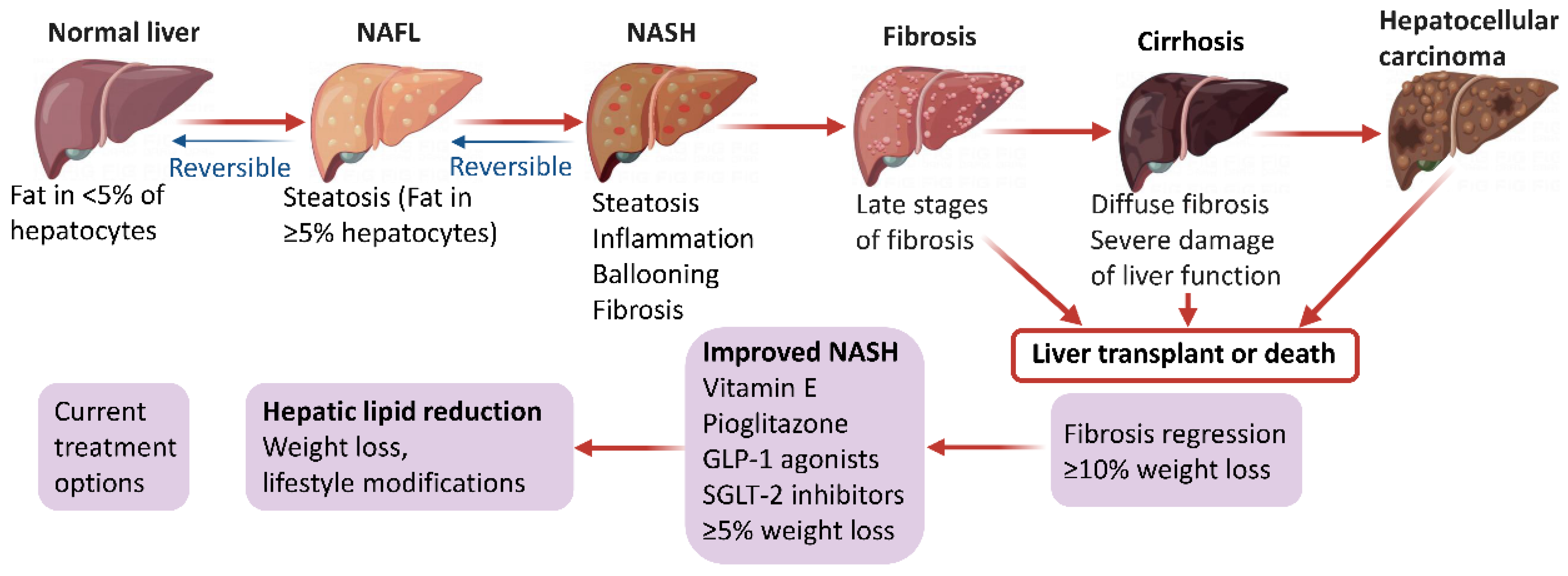
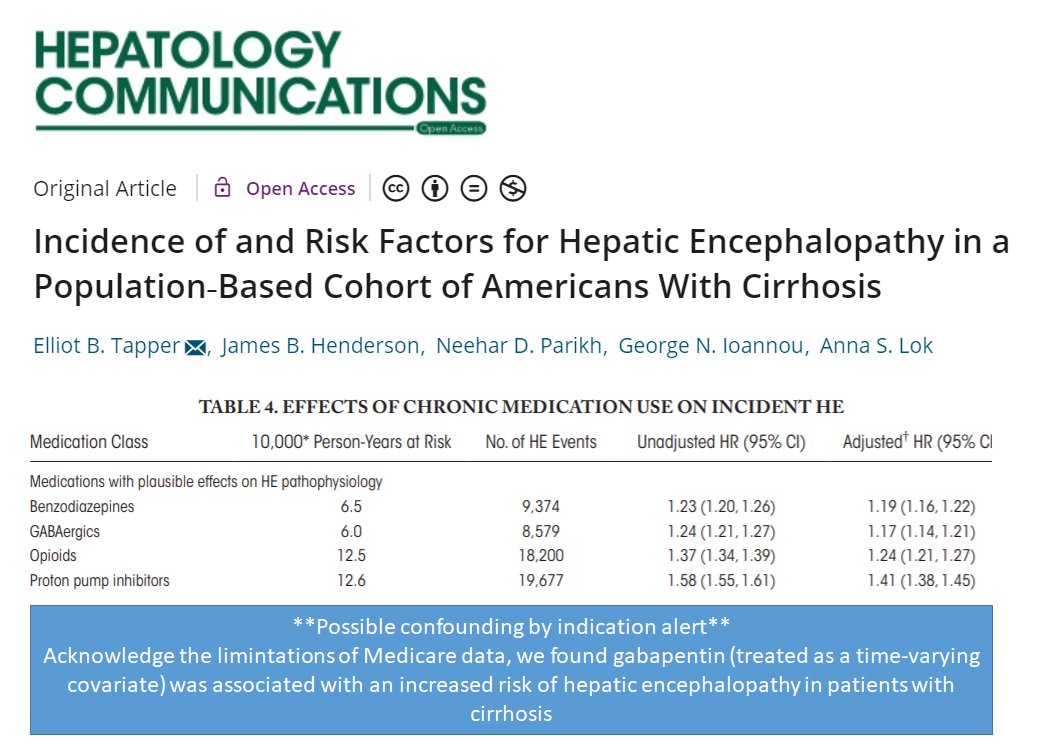
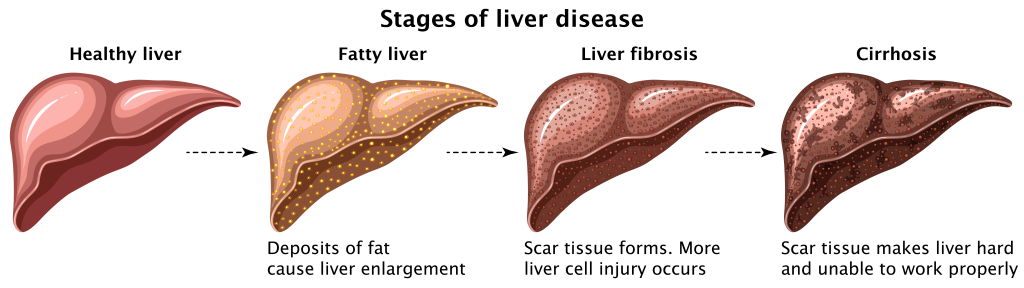
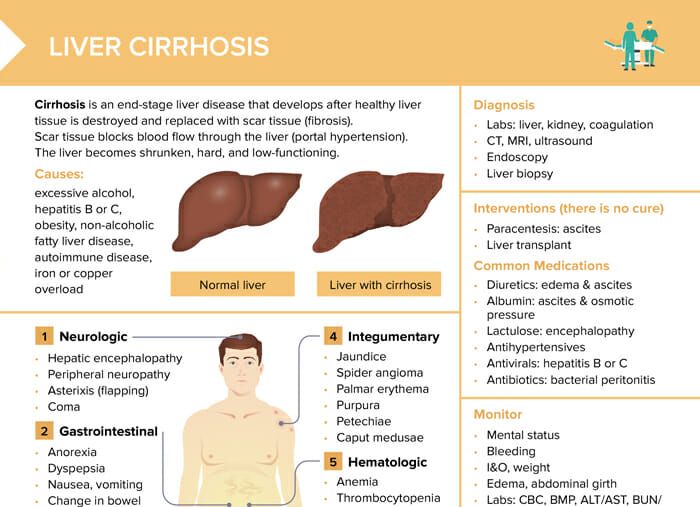
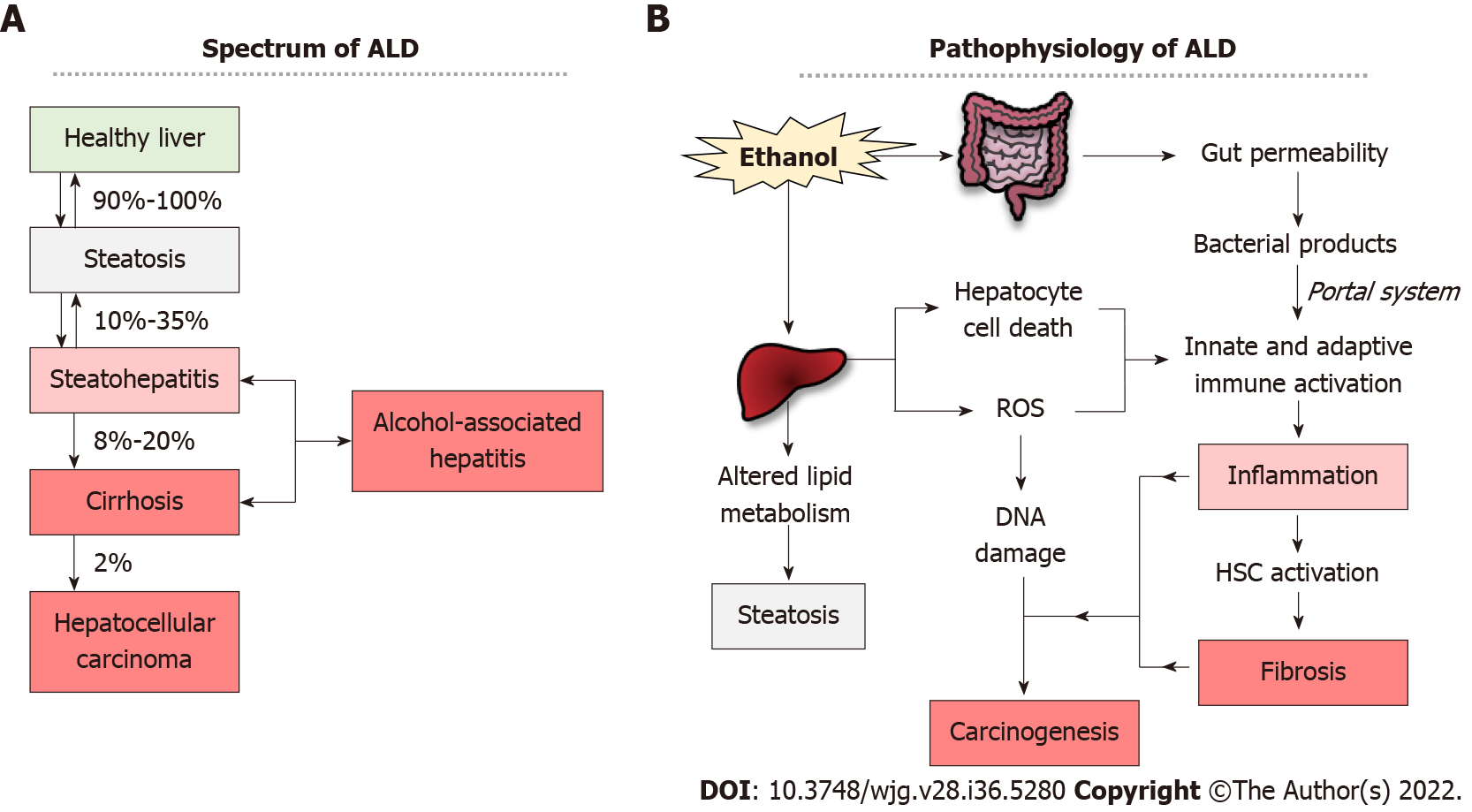
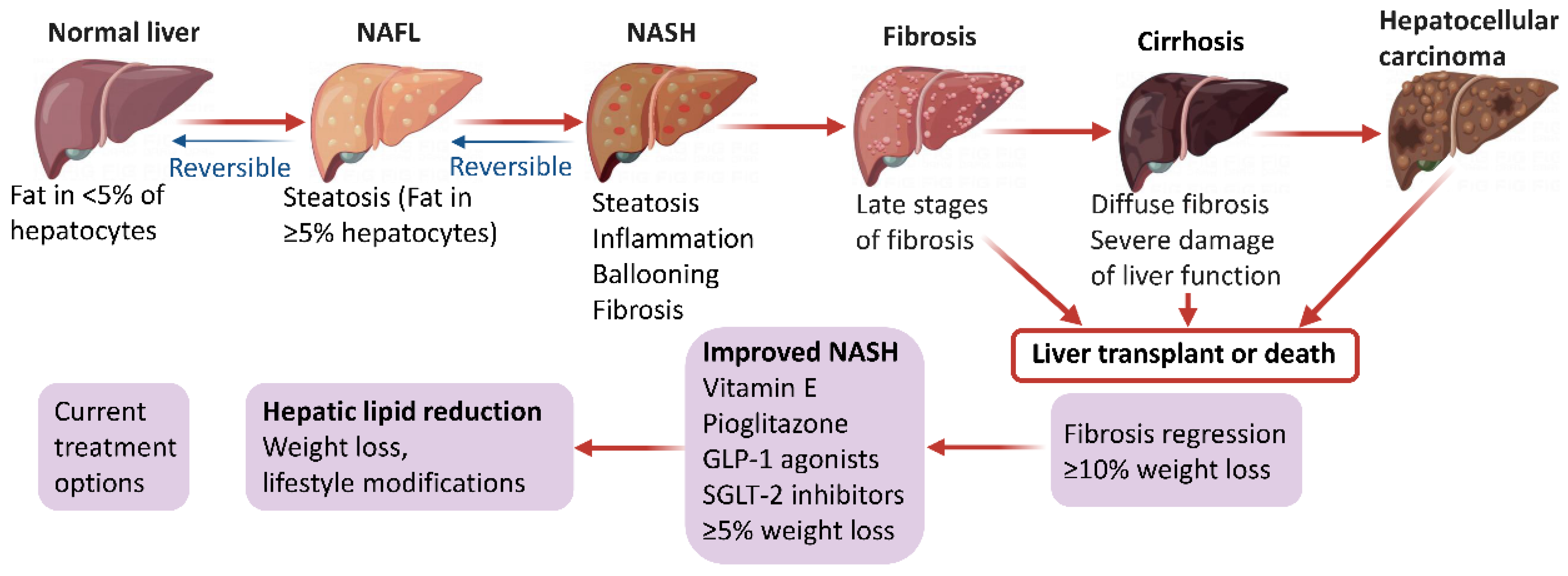
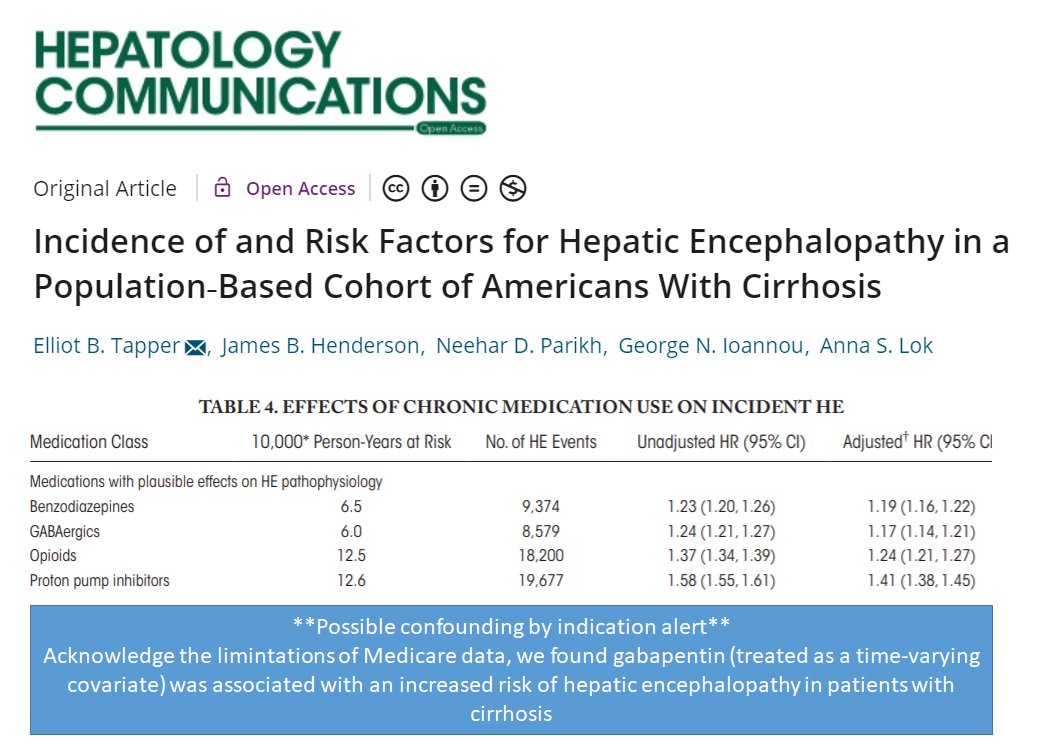
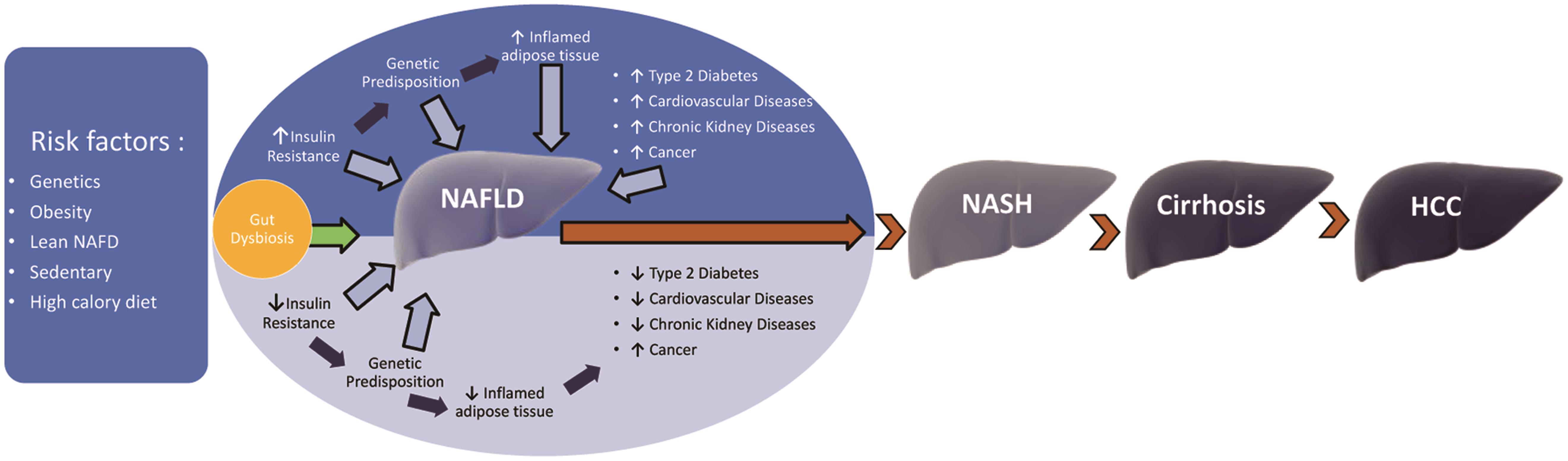
Gabapentin/pregabalin: not metabolized by the liver or bound by proteins, but consider renal dysfunction in cirrhosis patients, as well as other relevant side effects (e.g. sedation, dizziness); minimal data on safety of these agents. Pre-existing liver conditions, such as cirrhosis or hepatitis, could potentially increase the risk associated with gabapentin. While gabapentin isn't directly metabolized by the liver to a significant extent, any impairment could affect how your body processes medications in general. Pain is prevalent in patients with cirrhosis. Due to potential alterations in drug metabolism, risk for adverse effects, and complications from cirrhosis, physicians are often faced with difficult choices when choosing appropriate analgesics in these patients. Overall, acetaminophen remains the preferred analgesic. Despite its potential for intrinsic liver toxicity, acetaminophen is safe when Gabapentin is generally considered safe for the liver, but rare cases of liver damage have been reported. Gabapentin, a medication primarily used to treat nerve pain and seizures, has gained popularity for its effectiveness and relatively mild side effects. Nonetheless, due to their minimal hepatic metabolism and rarity of drug-induced liver injury, gabapentin and pregabalin can likely be used safely in patients with cirrhosis. The liver is responsible for the selective uptake, concentration, metabolism, and excretion of most drugs. Both prescription and over-the-counter medications can cause hepatotoxicity through a variety of mechanisms. Measures such as drug dose adjustment can help prevent adverse drug reactions in patients with cirrhosis. The choice of analgesic agent in cirrhotic patients is problematic and must be individualized taking into account several factors including severity of liver disease, history of opioid dependence, and potential drug interactions. With a cautious approach including slow dose up-titration and careful The treatment of pain in patients with cirrhosis is complicated by unpredictable hepatic drug metabolism and a higher risk of adverse drug reactions. We aimed to conduct a scoping review regarding pain management in cirrhosis. Despite the high Gabapentin, a gamma-aminobutyric acid (GABA) analogue, has infrequently been reported to cause liver injury; however, the causality in the previous reports is contested. Herein, we report a gabapentin-induced hepatocellular injury in a patient without another identifiable cause for acute liver injury. Pain management in patients with cirrhosis is a difficult clinical challenge for health care professionals, and few prospective studies have offered an evidence-based approach. In patients with end-stage liver disease, adverse events from analgesics are frequent, potentially fatal, and often avoidable. Severe complications from analgesia in these patients include hepatic encephalopathy Pain management in patients with cirrhosis is a difficult clinical challenge for health care professionals, and few prospective studies have offered an evidence-based approach. In patients with end-stage liver disease, adverse events from analgesics Cirrhosis is defined as permanent liver fibrosis secondary to damage or injury. It is a heterogeneous diagnosis, resulting in varying degrees of nodule formation, organ dysfunction, complications, and significant morbidity and mortality. Gabapentin is eliminated through the kidneys and, therefore, doesn’t typically cause liver injury. Learn safe dosage recommendations for people with liver disease. Unique Concerns in Patients With Cirrhosis In patients with cirrhosis, liver dysfunction leads to alterations in drug pharmacokinetics and metabolism (Fig. 2), which can lead to an increased risk for hepatotoxicity and accumulation of toxic metabolites. 2 Table 1 summarizes the unique management considerations in this population. Figure 2. Nonetheless, due to their minimal hepatic metabolism and rarity of drug-induced liver injury, gabapentin and pregabalin can likely be used safely in patients with cirrhosis. اپتوديت بزرگترين و قابل اعتمادترين مرجع دادههاي مبتني بر شواهد (EBM-Evidence Base Medicine) علوم پزشکي و دارويي ميباشد.تجربه بيش از 5000 پزشک و شامل 8800 موضوع Unique Concerns in Patients With Cirrhosis In patients with cirrhosis, liver dysfunction leads to alterations in drug pharmacokinetics and metabolism (Fig. 2), which can lead to an increased risk for hepatotoxicity and accumulation of toxic metabolites. 2 Table 1 summarizes the unique management considerations in this population. Adverse outcomes associated with chronic pain in patients with cirrhosis. Chronic pain, including nociceptive pain, neuropathic pain, and nociplastic pain (along with associated symptoms), 9 is correlated with high rates of opioid 25 and gabapentin 19 prescription in patients with cirrhosis. Both opioid and gabapentinoid use are correlated with poor functional status and quality of life, 3–6 Introduction The management of pain in the patient with cirrhosis is difficult, and the risk of an adverse event is high. Clinical scenarios including opioid dependence, postoperative pain management, palliative care in advanced hepatocellular carcinoma, and neuropathic pain syndromes can be a clinical challenge to the most experienced physician. Much of the apprehension stems from the risk of Adverse outcomes associated with chronic pain in patients with cirrhosis. Chronic pain, including nociceptive pain, neuropathic pain, and nociplastic pain (along with associated symptoms), 9 is correlated with high rates of opioid 25 and gabapentin 19 prescription in patients with cirrhosis.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | |
 |  |