Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
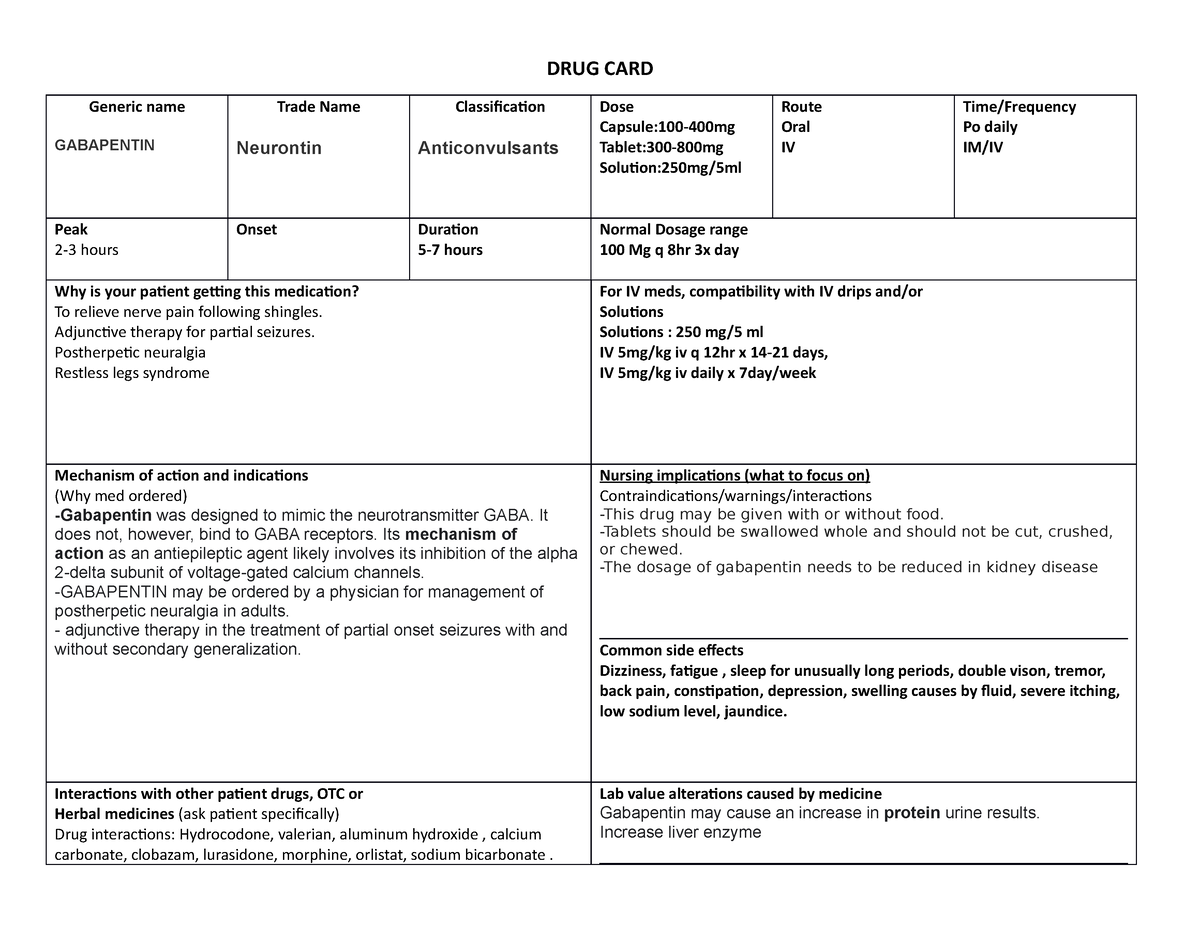
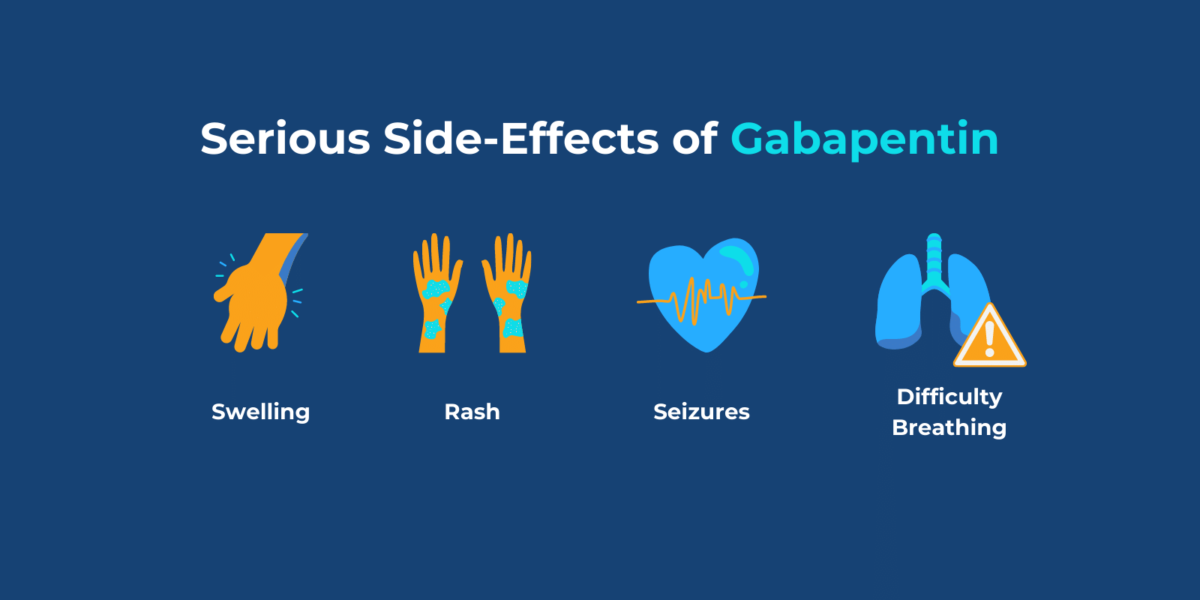
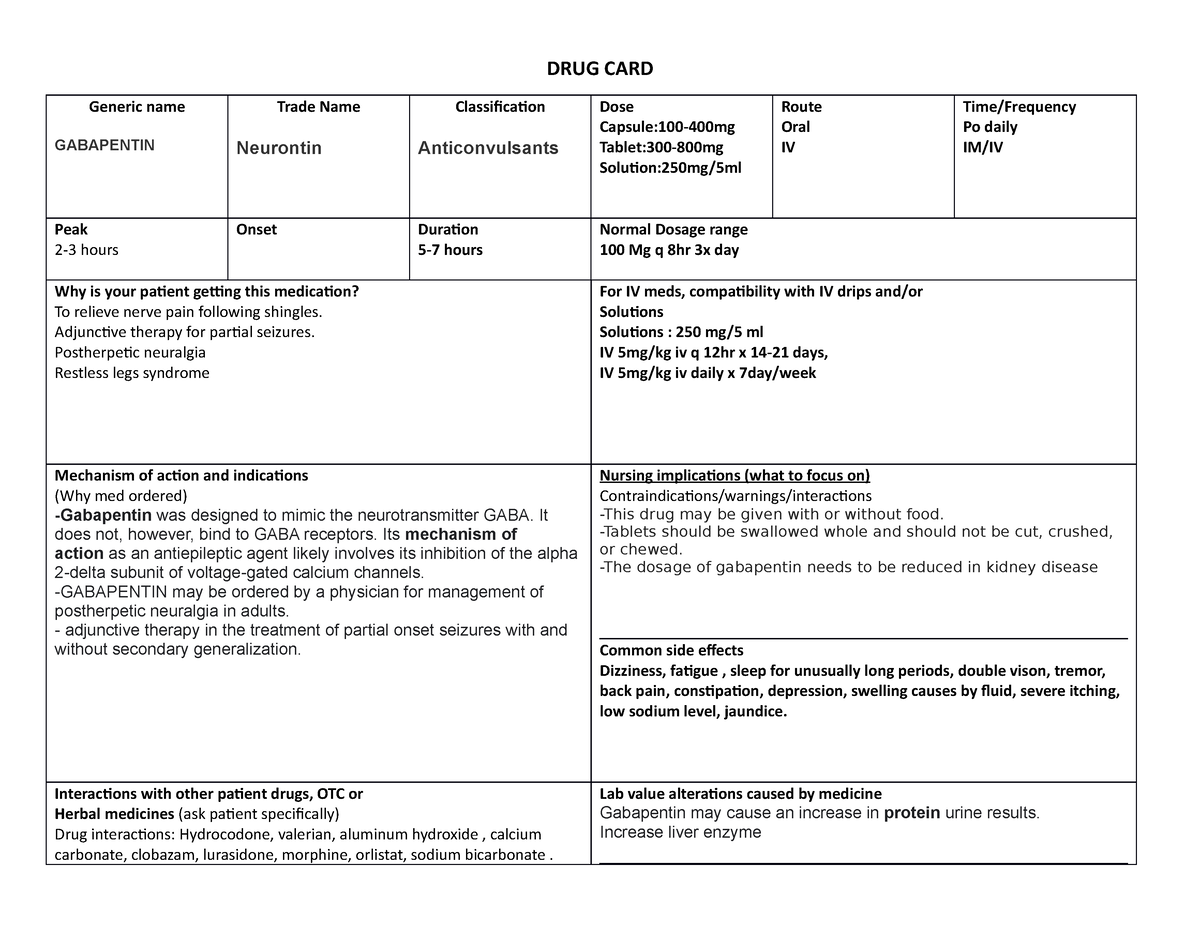
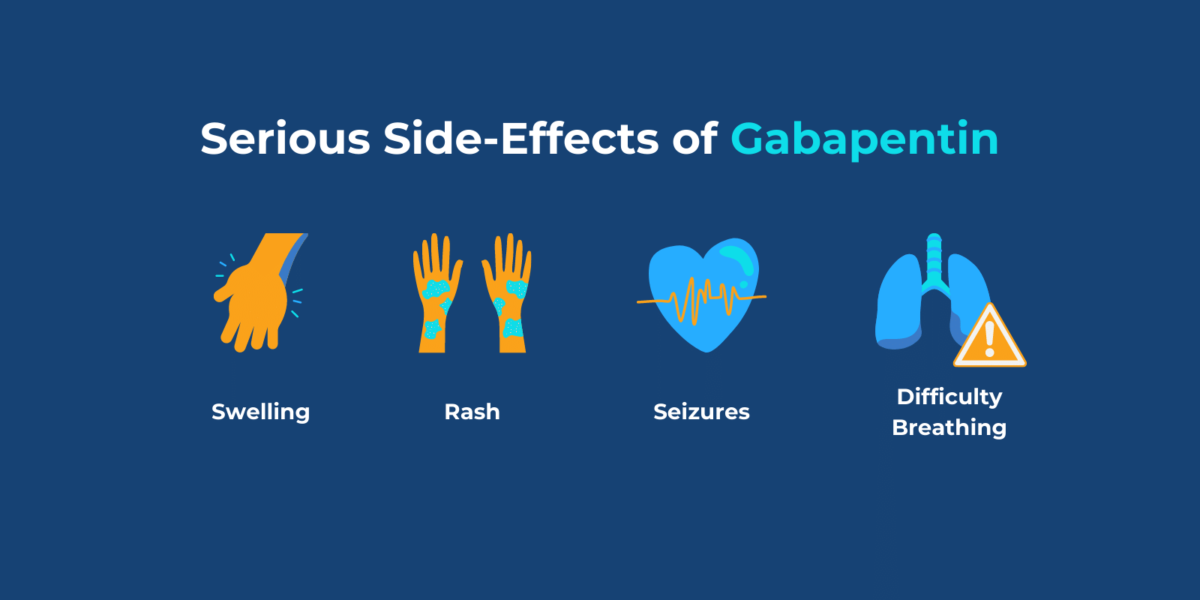
Sympathomimetic toxicity (cocaine, amphetamine, ketamine) Anticholinergic toxicity Heat stroke Delirium tremens Hypothalamic stroke Pheochromocytoma Thyroid storm Treatment Consider GI decon with Activated Charcoal if patient presents <2 hours after ingestion and remains cooperative Sedation Decreases the risk of hyperthermia, rhabdo, traumatic Max dosage 3600mg if patient already on gabapentin Taper dose > 7 days to discontinue [1] Pediatric Dosing Partial seizures Adjunct for partial seizures with out secondary generalization in patients> 12yo with epilepsy; also adjunctive therapy for partial seizures in patients 3-12 years <3 years: Safety and efficacy not established Max dosage 3600mg if patient already on gabapentin Taper dose > 7 days to discontinue [1] Pediatric Dosing Partial seizures Adjunct for partial seizures with out secondary generalization in patients> 12yo with epilepsy; also adjunctive therapy for partial seizures in patients 3-12 years <3 years: Safety and efficacy not established Overdose with newer anticonvulsant agents include: Gabapentin, Lamotrigine, Levetiracetam, Oxcarbazepine, Pregabalin, Tiagabine, Topiramate and Vigabatrin. Comprehensive guide on overdose management, including symptoms, diagnosis, and treatment options for various substances. Essential resource for healthcare professionals. UpToDate UpToDate There is no fatal dose of gabapentin, as everyone has different factors that affect how much of the drug is appropriate – and how much can cause an overdose. Your weight, age, gender, and individual health history can factor into your doses so that an overdose can occur at much higher or lower doses for some people compared to others. Expert opinion: Loperamide, gabapentin, and modafinil are becoming drugs of abuse, and as such, should be on the radar of healthcare providers. Recognizing their unique toxicity profiles is imperative in providing optimal resuscitative care. Keywords: Evidence-based emergency medicine; gabapentin; loperamide; modafinil; toxicology. Objective: To raise awareness of serious toxicity, including respiratory depression and PRES (posterior reversible encephalopathy syndrome) caused by gabapentin in the setting of overdose and abuse. Background Gabapentin, a structural analog of γ-aminobutyric acid, although developed for epilepsy, is often used for pain, insomnia and anxiety. The United States Centers for Disease Control Division of Overdose Prevention has reported that toxicology tests identified gabapentin in 10% of deaths due to drug overdose in 2019 and 2020. Gabapentin is licensed in the US for the treatment of postherpetic neuralgia and is widely used to treat other types of neuropathic pain. It is used illicitly to potentiate the effects of opioids, a A case report of a gabapentin overdose describes a 16 vear- old girl who presented to the emergency department 8 hours status post reportedly ingesting 48.9 grams (860 mg/kg) of gabapentin (163 capsules of the 300 mg gabapentin formulation). At 6 hours post ingestion, the girl complained of dizziness and also diarrhea that had occurred during General Type: Anticonvulsants; GABA analog Dosage Forms: capsule, tablet, oral solution 250mg/5mL Common Trade Names: Neurontin, Gralise Postmortem toxicology tests detected gabapentin in almost 1 in 10 US overdose deaths between 2019 and 2020. In about half of the cases, a medical examiner or coroner ruled the drug was a cause of the death, according to a report from the CDC’s Division of Overdose Prevention. The percentage of deaths with gabapentin detected that were opioid-involved remained consistently high, ranging from 85% to 90%. Illicit opioid-involved deaths accounted for 56.8% of overdose deaths with gabapentin detected in the first quarter of 2019 and 69.2% in the last quarter of 2020; this increase was largely driven by illicitly manufactured fentanyl and fentanyl analogs. The percentage Baclofen toxicity Opioids Lomotil toxicity Loperamide toxicity Toxic alcohols Ethanol Ethylene glycol Isopropyl alcohol Methanol Xylazine toxicity Evaluation Urine toxicology screen Most benzodiazepine screens look for oxazepam, which is a metabolite of diazepam and chlordiazepoxide. Therefore, lorazepam, alprazolam, and clonazepam are commonly Background Withdrawal symptoms due to reduced GABA and increased NMDA receptors Benzos useful due to cross tolerance at ethanol GABA receptor and longer half-life Symptom-triggered therapy As effective as fixed dose therapy, but with more rapid detox Don’t use phenytoin or fosphenytoin to treat seizures caused by drug toxicity or drug withdrawal. [1] Clinical Features Reduction in alcohol See Also Opioid overdose Opioid withdrawal Analgesics and Sedatives (Pediatrics) Complex regional pain syndrome References Adapted from Tintinalli and Harwood & Nuss, World Health Organization 3-Step Analgesia Ladder for Cancer & Washington Manual Intership Survival Guide, 2008 These medications can cause lethargy or agitation in overdose, increase risk of death combined with opioids, and manifest a withdrawal syndrome. This topic will discuss the evaluation and management of gabapentinoid poisoning and withdrawal. A summary table to facilitate emergency management is provided (table 1). Toxicity from gabapentin and pregabalin overdose is commonly encountered. Treatment is supportive, and the use of extracorporeal treatments (ECTRs) is controversial. The EXTRIP workgroup conducted systematic reviews of the literature and summarized findings following published methods. Thirty-three articles (30 patient reports and 3 pharmacokinetic studies) met the inclusion criteria. High These medications can cause lethargy or agitation in overdose, increase risk of death combined with opioids, and manifest a withdrawal syndrome. This topic will discuss the evaluation and management of gabapentinoid poisoning and withdrawal. A summary table to facilitate emergency management is provided (table 1).
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |