Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
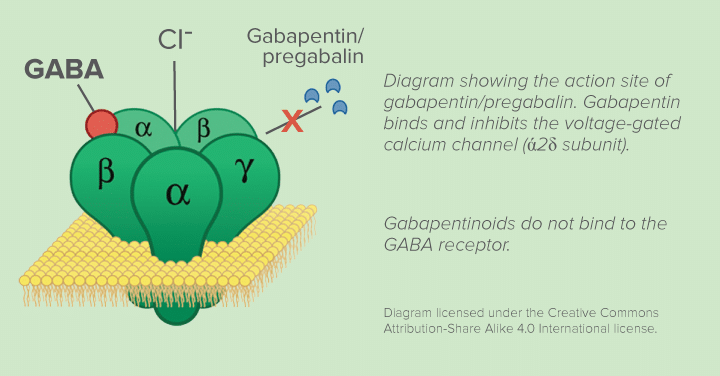 |  |
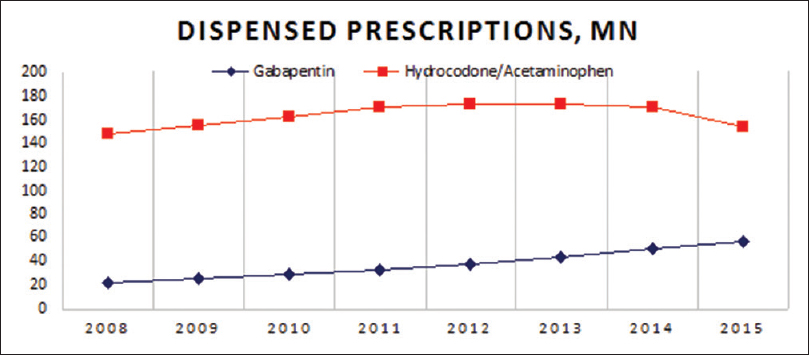
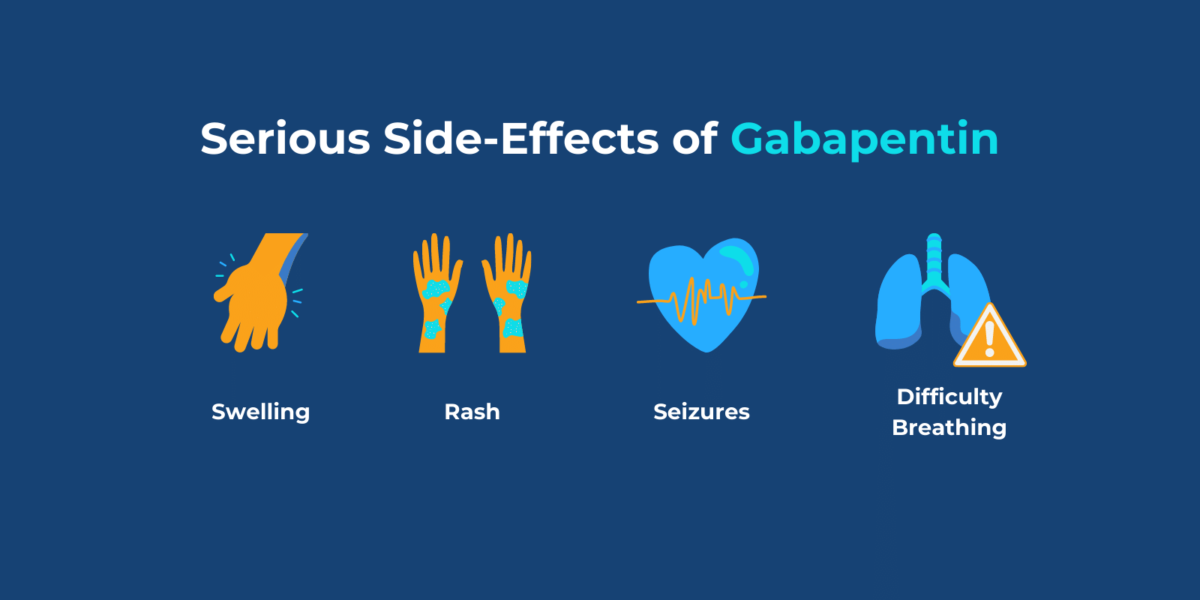
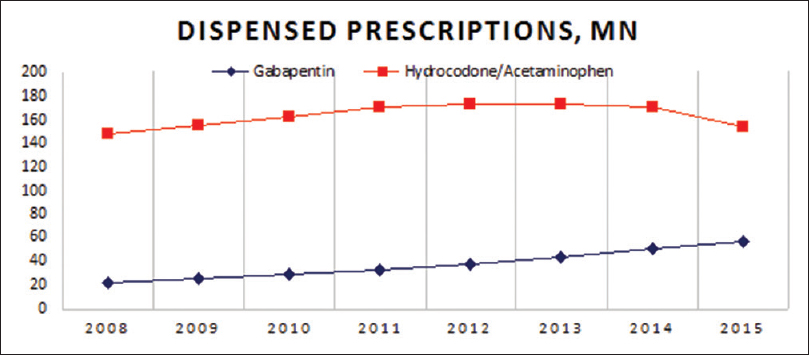
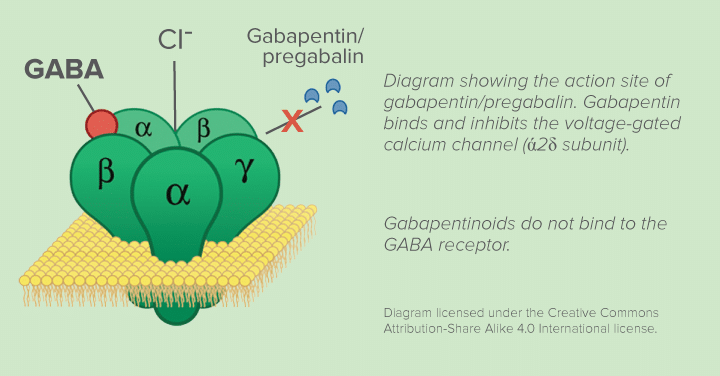
Abstract BACKGROUND: Gabapentin, an anticonvulsant, has recently been suggested as an effective postoperative ‘analgesic’ agent. The objective of the present study was to examine the analgesic effectiveness, opioid-sparing effects and side effects associated with the use of gabapentin in a perioperative setting. METHODS: Following the Quality of Reporting of Meta-analyses recommendations Perioperative gabapentin upped the risk of delirium, new antipsychotic use, and pneumonia in older adults after major surgery, a retrospective study showed. Gabapentin is an anticonvulsant medication prescribed for a variety of conditions. Learn about its uses, side effects, and what you should know if you've been prescribed this medication. This cohort study examines whether perioperative gabapentin use among older adults after major surgery is associated with in-hospital adverse clinical events. Conclusion: The preoperative administration of gabapentin appears to be an effective strategy for enhancing postoperative pain control and reducing opioid use in orthopedic patients undergoing spinal anesthesia. Further studies are necessary to determine the optimal dosing regimen and long-term effects of gabapentin in this setting. Gabapentin may be prescribed either before or after surgery to help with postsurgical pain. However, it should be used with caution due to the high risk of abuse. This cohort study examines whether perioperative gabapentin use among older adults after major surgery is associated with in-hospital adverse clinical events. For individuals preparing for surgery, managing pain effectively can be crucial for recovery. However, the use of Gabapentin before surgical procedures raises questions about its safety and efficacy in that context. The primary concerns revolve around potential interactions with anesthesia and other medications administered during surgery. Results While patients 65 years and older who received gabapentin were found to experience fewer adverse effects than nonusers prior to propensity score matching, afterward they were found to be at increased risk of delirium, new antipsychotic use, and pneumonia when compared to gabapentin nonusers after major surgery. In this cohort study, perioperative gabapentin use was associated with increased risk of delirium, new antipsychotic use, and pneumonia among older patients after major surgery. These results suggest careful risk-benefit assessment before prescribing gabapentin for perioperative pain management. Abstract Purpose of review: This review summarizes the risks and benefits of gabapentinoids (gabapentin and pregabalin) for perioperative pain control and the controversies surrounding their use in a variety of settings. We review current literature with the goal of providing patient-centric and procedure-specific recommendations for the use of these medications. While the use of gabapentin may reduce pain and spare opioids in younger populations, the risks in older adults do not seem to outweigh the benefits. As a health care system, we need to strategize more broadly about pain control after surgery. Making progress in this complex clinical space is not easy, but improvements are achievable. Gabapentin treats epilepsy and nerve pain. Recently, it’s been used after bariatric surgery to manage pain. So, what should patients know about taking it post-surgery? This article will discuss the benefits and risks. We’ll cover its impact on weight loss, side effects, and key points for patients and doctors. Would you want to take Lyrica (pregabalin) or Neurontin (gabapentin) for pain relief after a major surgery? Both drugs belong to a class of nerve medication called gabapentinoids that are increasingly being prescribed to patients perioperatively (after surgery) as an alternative to opioid medication. While more research studies point to the increased effectiveness of pain management in patients undergoing bariatric surgery with an adjuvant use of gabapentin, some data show risks associated with using gabapentinoids like gabapentin. Turan et al. investigated the effects of gabapentin on acute postoperative pain and on morphine consumption in patients undergoing spinal surgery where 1,200 mg gabapentin was given 1 hour before surgery. Understanding Gabapentin Dosage Dosage can vary significantly from one patient to another. Typically, gabapentin is started at a low dose and gradually increased until effective pain relief is achieved or side effects become intolerable. The standard starting dose after surgery might range from 300 mg to 600 mg per day, divided into three doses. It’s crucial to monitor how each person Effective postoperative pain management is crucial in the care of surgical patients. Opioids, which are commonly used in managing postoperative pain, have a potential for tolerance and addiction, along with sedating side effects. Gabapentin’s use as A study of laparoscopic cholecystectomy included in the analysis used a dose of 300 mg. They found that gabapentin resulted in a 35% reduction in total analgesic consumption in the first 24 hours following surgery. Gabapentin also resulted in 27% to 39% reduction in visual analog scale (VAS) pain scores in the first 24 hours postoperatively. We defined which procedures most commonly had gabapentin prescribed postoperatively, and the unadjusted risk of prolonged use for each medication category and for type of surgery. Additionally, we assessed concomitant prolonged use of opioids since that can increase the risk of adverse drug events (Supplementary Appendix4).
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |