Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 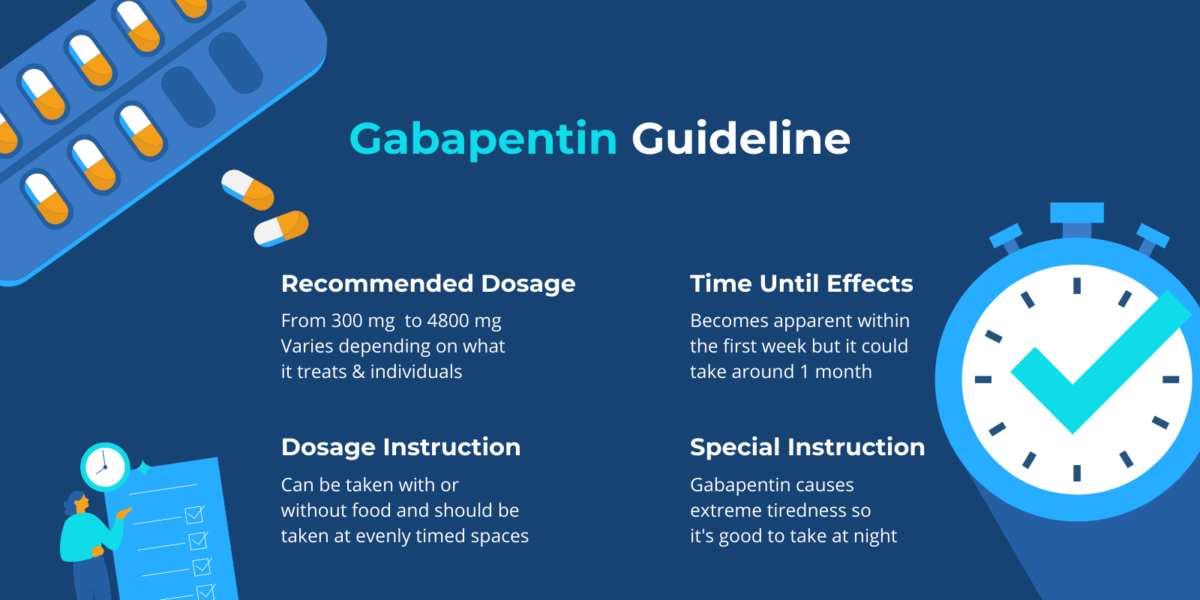 |
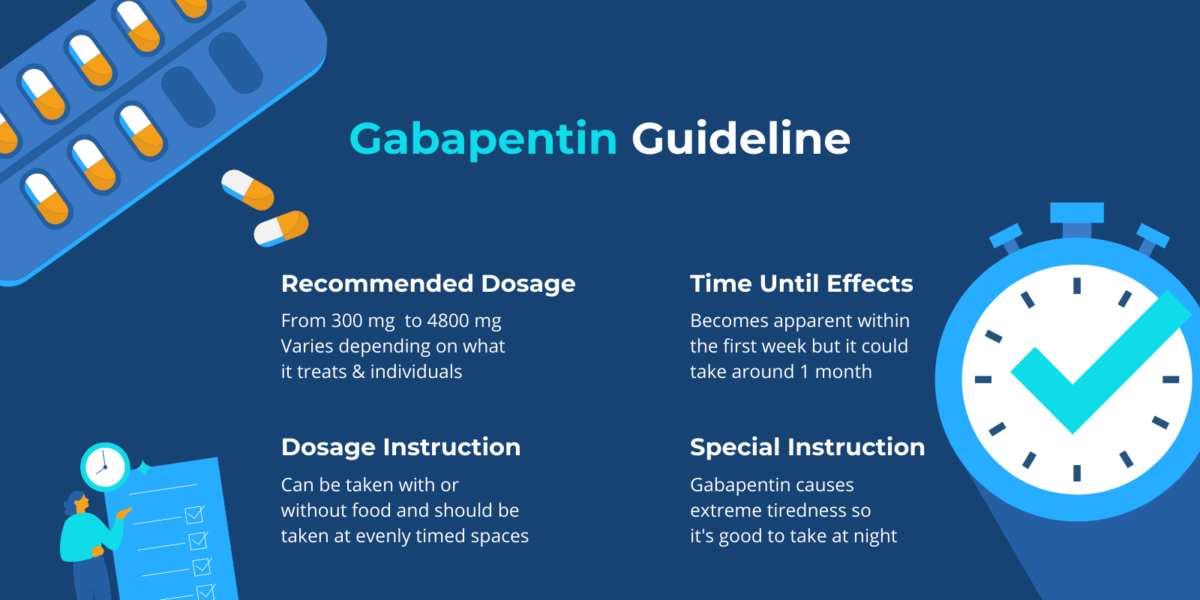
Abstract Purpose of review: Gabapentinoids are frequently used in the management of cancer pain. In recent Cochrane systematic reviews, although there was an abundance of evidence relating to non-cancer pain, only a few studies related to cancer pain. This review summarizes recent randomised controlled trials (RCTs) evaluating the use of gabapentinoids for tumour-related (as monotherapy or Given the significant benefits of gabapentin and the combination of gabapentin with opioids for the treatment of neuropathic pain, randomized clinical trials are needed to establish the role of these analgesic regimens for the treatment of neuropathic cancer pain. Adults diagnosed with chronic low back pain were included; those with prior gabapentin use, dementia, epilepsy, stroke, or cancer were excluded. Propensity score matching controlled for demographics, comorbidities, and pain medications. Patients. Seventy-five cancer patients who had previously received chemotherapy, and had experienced at least one symptom of neuropathic pain were included in the intervention group. They received a fixed low-dose of gabapentin (800 mg/day). Abstract Background: Gabapentin has been evaluated in the treatment of nonmalignant neuropathic pain, however, there is little direct evidence evaluating its efficacy in cancer-related neuropathic pain. BACKGROUND: Gabapentin (GBP), originally an antiepileptic drug, is more commonly used in the treatment of neuropathic pain. In recent years, GBP has been used as an adjunct or primary therapy in non-neuropathic pain, most commonly for the treatment of perioperative and cancer pain. Gabapentin, which belongs to the class of medications called anticonvulsants, treats seizures by decreasing excitement in the brain. Gabapentin has been studied for its effect in patients with cancer who have neuropathic pain or symptoms of peripheral neuropathy. The drug changes the way the body senses pain. Their discovery, published today in JAMA Network Open, suggests that a prophylactic, or preventative, gabapentin dose of 3600 mg daily can delay or eliminate the need for opioids to manage the pain associated with radiation-induced oral mucositis in patients with head and neck cancer. In the context of cancer, gabapentin is often used to manage cancer-related pain, particularly neuropathic pain. This type of pain can result from the cancer itself or as a side effect of treatments like chemotherapy, radiation therapy, or surgery. Gabapentin can help improve the quality of life for cancer patients by reducing pain and discomfort. The main aim of this study was to determine whether gabapentin, a common adjuvant analgesic in current use against cancer-associated neuropathic pain, would affect tumour development and progression in vivo. The Dunning rat model of prostate cancer was used. Abstract Purpose This review was designed to compile the currently available evidence on the prophylactic use of gabapentin in the head and neck cancer patient population. Methods A systematic search was conducted of PubMed, Web of Science, and Google Scholar to identify articles related to the use of prophylactic gabapentin in patients undergoing head and neck cancer therapy. Candidate Gabapentin, which affects voltage-gated calcium channels in the brain, was originally approved as an anti-seizure medication and later for treating nerve pain. Today, up to 95% of its use may be "off-label," researchers have found — highlighting a lack of rigorous study of its mechanisms and efficacy for treating pain more broadly, as well as other conditions it's commonly prescribed for More than 30% of cancer patients experience neuropathic pain. Opioids, as standard pain-relief agents, cannot achieve satisfactory outcomes to treat neuropathic cancer pain due to drug resistance and side effects. Meanwhile, gabapentin, a We report three cases of cancer pain, treated with primary cancer from the prostate metastasis to the spine. All three patients had lower back pain that radiated to the left and right limbs, with mixed pain and bone pain, where early hospital admission shows the Numeric Rating Scale (NRS) pain scale 9–10. Treated with administration of adjuvant therapy (Gabapentin) and weak opioids Breakthrough Cancer Pain (BTcP) is defined as a temporary increase in pain that occurs spontaneously. The use of gabapentin is believed to be able to reduce pain complaints in patients with BTcP. However, research to support the efficacy of The effects of Gabapentin are well-known in conditions such as post-herpetic neuralgia, painful diabetic neuropathy, spinal cord injury pain, and neuropathic cancer pain. More common cancer-related neuropathic pain syndromes are listed in Table 1. The use of Gabapentin in patients with neuropathic pain can alleviate pain and increase daily Between 2005 and 2015, prescriptions for gabapentinoid medications -- gabapentin and pregabalin -- to adults with cancer saw a two-fold increase, a U-M Rogel Cancer Center study has found. The main aim of this study was to determine whether gabapentin, a common adjuvant analgesic in current use against cancer-associated neuropathic pain, would affect tumour development and progression in vivo. The Dunning rat model of prostate cancer was used. This comparative-effectiveness study uses data from 2 clinical trials to evaluate whether the use of gabapentin for pain management is associated with less opioid use and feeding tube placement among adult patients with head and neck cancer receiving chemoradiotherapy. Methods We present the cases of four patients who were effectively treated with gabapentinoids for refractory rectal/vesical tenesmus induced by malignant tumors. Therefore, patients who were effectively treated with pregabalin or gabapentin for rectal and vesical tenesmus after ineffective treatment with opioids at the National Cancer Center Hospital between April 2009 and March 2014 were
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |