Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 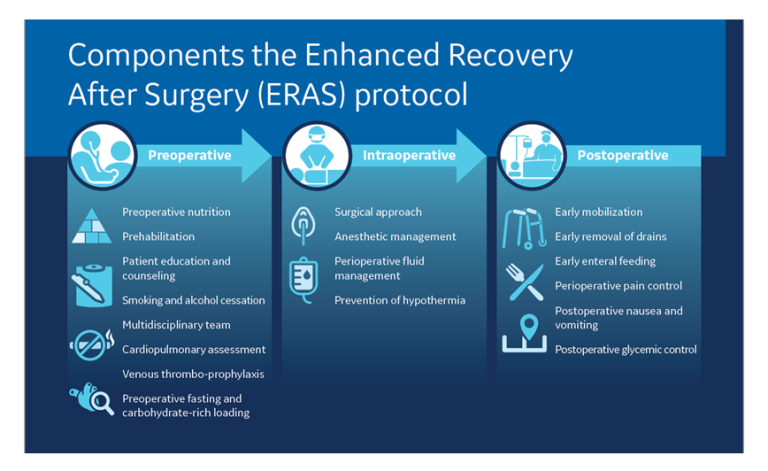 |
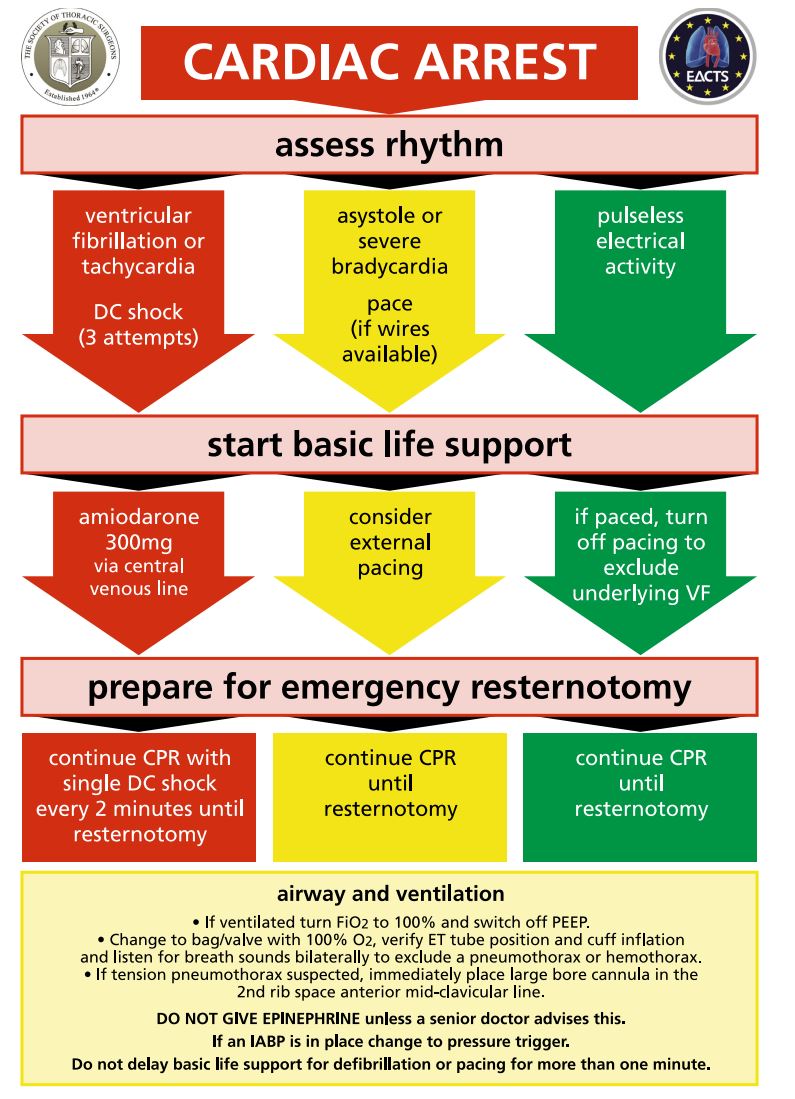
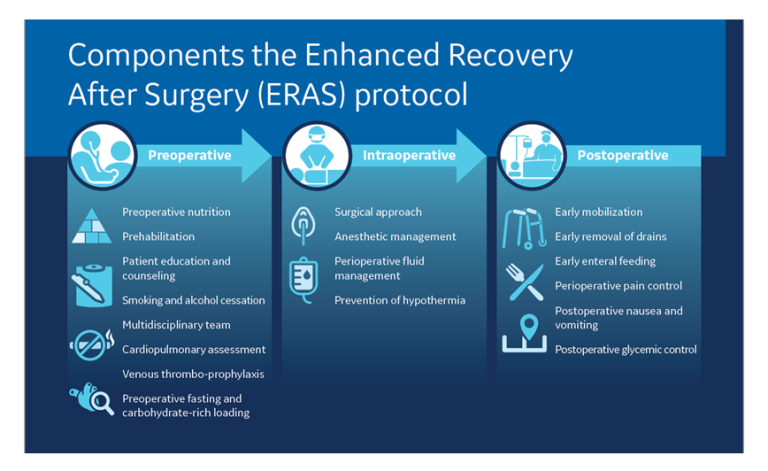
Objectives: The purpose of this study was to evaluate the analgesic effects of perioperative gabapentin on postopera-tive acute and chronic pain after coronary artery bypass graft (CABG) surgery with median sternotomy and internal mammary artery harvesting. This study evaluated whether perioperative administration of gabapentin in cardiac surgery patients could reduce postoperative opioid consumption, postoperative sleep or perceived quality of recovery. This randomised controlled trial assigned 60 patients undergoing cardiac surgery to receive 1200 mg of gabapentin or placebo two hours preoperatively, and then 600 mg of gabapentin or placebo Gabapentin significantly reduced the intensity of pain and tramadol consumption in the early postoperative period after CABG surgery. Pain scores at 1 and 3 months after surgery were low in both groups, with no significant difference between the groups. Enhanced Recovery After Surgery protocols are relatively new in cardiac surgery. Enhanced Recovery After Surgery addresses perioperative analgesia by implementing multimodal pain control regimens that include both opioid and nonopioid components. We investigated the effects of an Enhanced Recovery After Surgery protocol at our institution on postoperative outcomes with particular focus on As neuropathic pain is a significant component here, gabapentin and pregabalin may be effective in these patients and may reduce postoperative opioid consumption. The purpose of this systematic review was to find out efficacy of gabapentin and pregabalin in acute postoperative pain after cardiac surgery. Conclusions: Gabapentin appears safe and well tolerated when used for persistent post-operative and post-traumatic pain in thoracic surgery patients, although minor side effects do occur. Gabapentin may relieve refractory chest wall pain in some of these patients, particularly those with more severe pain. The shift towards multimodal pain regimens, including gabapentin, has taken place without attention to ensuring that they, like opioids, are appropriately discontinued soon after surgery. The prevalence of prolonged use of post-operative gabapentin among older adults is unknown, as are the factors associated with prolonged use. Oral GABA at a dose of 600 mg given before cardiac surgery significantly reduced postoperative morphine consumption and postoperative pain both at rest and with cough. Patients undergoing cardiothoracic surgery are exposed to opioids in the operating room and intensive care unit and after hospital discharge. Opportunities exist to reduce perioperative opioid use at all stages of care and include alternative oral Enhanced Recovery After Surgery protocols are relatively new in cardiac surgery. Enhanced Recovery After Surgery addresses perioperative analgesia by implementing multimodal pain control regimens that include both opioid and nonopioid components. We Rapchuk, I. L., et al. (2010). "Effect of gabapentin on pain after cardiac surgery: a randomised, double-blind, placebo-controlled trial." Anaesthesia and Intensive Care 38 (3): 445-451. This study evaluated whether perioperative administration of gabapentin in cardiac surgery patients could reduce postoperative opioid consumption., postoperative sleep or perceived quality of recovery. This INTRODUCTION The immediate postoperative period after cardiac surgical procedures such as coronary artery bypass grafting and valve replacements is characterized by a pattern of myocardial injury and recovery. Understanding this pathophysiology allows anticipation of physiologic derangements and early recognition and avoidance of complications. This topic discusses routine postoperative care This randomised controlled trial assigned 60 patients undergoing cardiac surgery to receive 1200 mg of gabapentin or placebo two hours preoperatively, and then 600 mg of gabapentin or placebo twice a day for the next two postoperative days. Postoperative opioid use was measured by the amount of fentanyl used in the first 48 hours postoperatively. The purpose of this study was to evaluate the analgesic effects of perioperative gabapentin on postoperative acute and chronic pain after coronary artery bypass graft (CABG) surgery with median sternotomy and internal mammary artery harvesting. Persistent postoperative pain (PPP) after cardiac surgery is a significant complication that negatively affects patient quality of life and increases health care system burden. However, there are no standards or guidelines to inform how to mitigate This review aimed to study the role of analgesia and sedation after coronary artery bypass graft (CABG) surgery, regarding pain management, assisted respiration, overall postoperative health care, and hospitalization. Data were collected from Abstract Background: One of the most common complaints after coronary artery bypass graft (CABG) is post-operative pain. Gabapentin is an anticonvulsant and antineuralgic agent. Objective: To evaluate the analgesic effect of preemptive gabapentin on post-operative pain and morphine consumption after cardiac surgery. Sleep architecture is frequently disrupted after major surgery, leading to acute and chronic postoperative sleep disorders that may contribute to episodic hypoxia, hemodynamic instability, postoperative fatigue, cognitive dysfunction, depression. These all have potentially detrimental impacts on disease regression. Pain is a key driver of postoperative sleep disruption and opioids are widely High dose gabapentin taper may be considered for patients with concomitant post-operative pain and alcohol withdrawal to decrease benzodiazepine use (see Alcohol Withdrawal Guideline) Patients on gabapentin prior to admission should be resumed on gabapentin, if clinically appropriate They used a gabapentin dose of 1.2 g per day treatment 1 hour before surgery and for 2 days after surgery and investigated its effect on postoperative acute pain.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |