Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
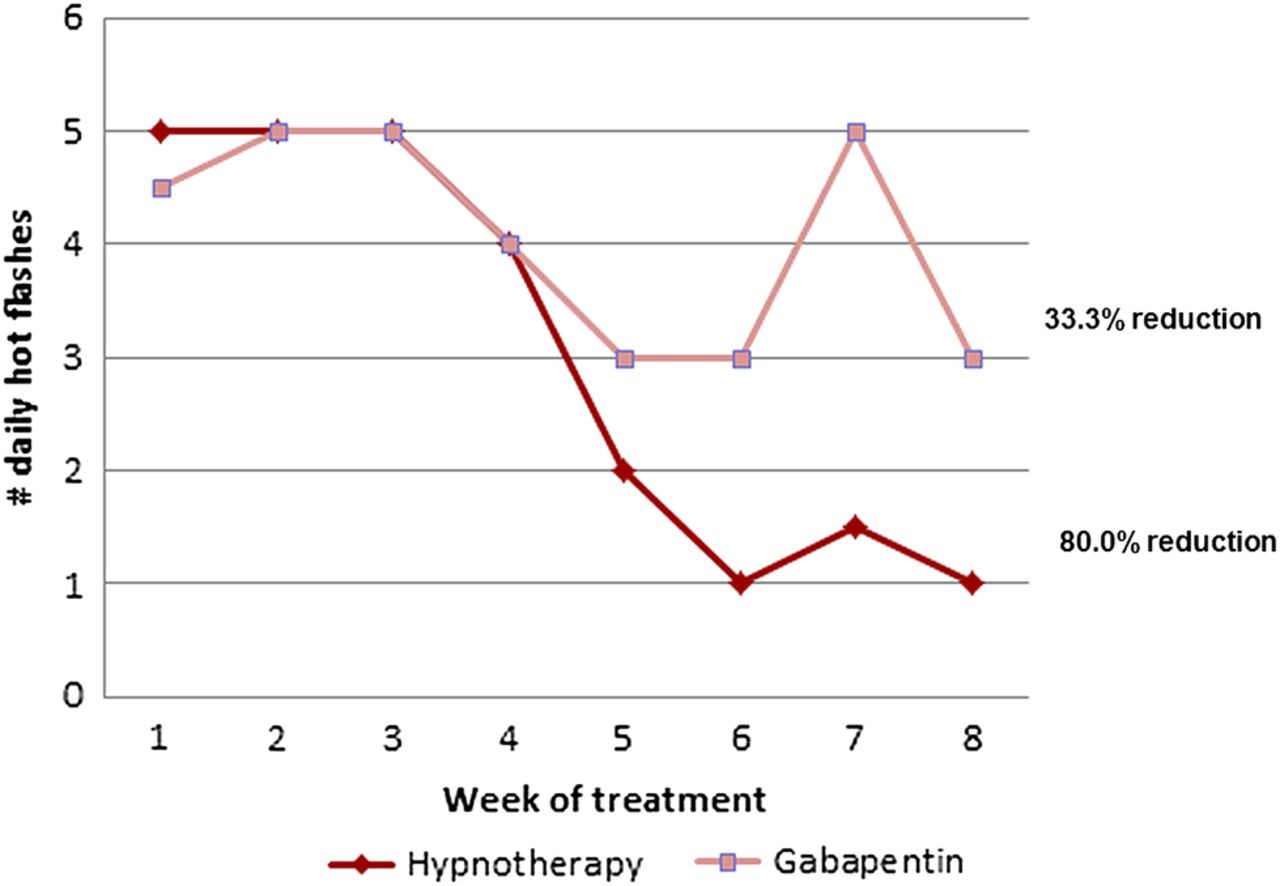
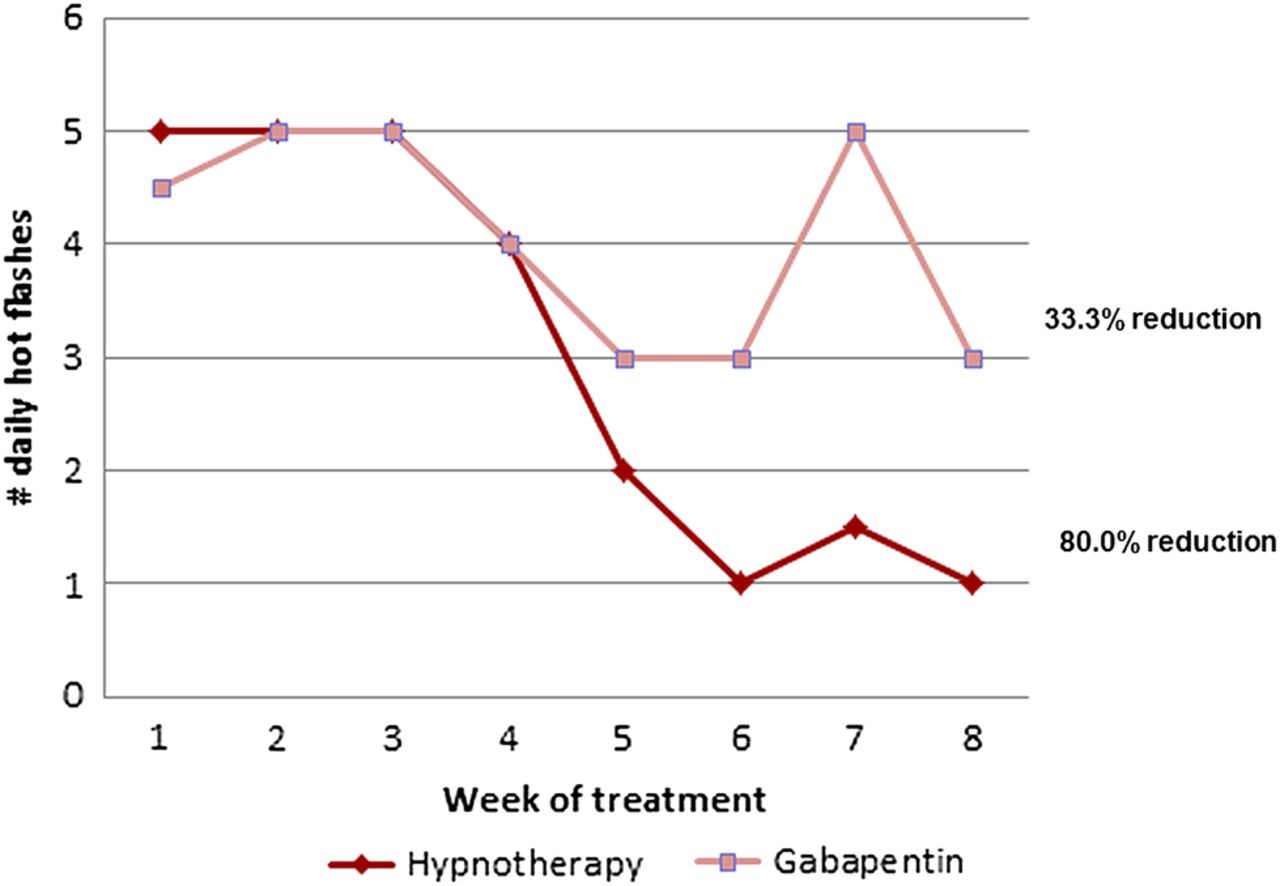
Hot flashes are a distressing symptom frequently experienced by survivors of breast cancer or prostate cancer who are receiving estrogen or androgen-deprivation therapies. The frequency and intensity of hot flashes can lead to diminished quality of life and decreased adherence with prescribed antineoplastic therapies. This evidence-based review synthesizes and updates the findings of the Gabapentin appears to be effective for the treatment of hot flushes with a favorable effect on quality of sleep. Vitamin E has only marginal effect on vasomotor symptoms. Gabapentin is effective in the control of hot flashes at a dose of 900 mg/day, but not at a dose of 300 mg/day. This drug should be considered for treatment of hot flashes in women with breast cancer. Hot flashes occur frequently in menopausal women and in women with breast cancer, diminishing their quality of life. A report from the Women's Health Initiative published in 2002 raised concerns about the long-term safety of estrogen therapy. Hot flashes can be a prominent problem in women with breast cancer. 1–3 In lieu of concerns regarding the use of hormonal therapies in these women, nonhormonal means of alleviating hot flashes are desirable. Purpose Hot flashes are a common and debilitating symptom among survivors of breast cancer. This study aimed at evaluating the effects of electroacupuncture (EA) versus gabapentin (GP) for hot flashes among survivors of breast cancer, with a specific focus on the placebo and nocebo effects. Hot flashes and night sweats can be cancer or treatment related and occur commonly in both women and men. Get information on hormonal and nonhormonal agents, cognitive and behavioral methods, and integrative medicine treatment options in this clinician summary. A 2005 study by Pandya et al. randomized 420 women with breast cancer and experiencing at least 2 hot flashes in 24 hours to one of three groups: gabapentin 300 mg daily, gabapentin 900 mg daily, or placebo 23. Centrally active agents (eg, venlafaxine, paroxetine, gabapentin) are regarded as the most promising nonhormonal treatments for hot flashes in breast cancer survivors. Nonpharmacologic and complementary alternative medicine therapies have limited effectiveness. Because the γ-aminobutyric analogue gabapentin (Neurontin) has been effective in controlling menopausal hot flashes, Pandya and colleagues studied the effectiveness of this medication in 420 women with breast cancer who were having two or more hot flashes per day were randomly assigned placebo, gabapentin 300 mg/day, or gabapentin 900 mg/day by mouth in three divided doses for 8 weeks. In a randomized, double-blind, placebo-controlled trial of gabapentin for hot flashes, 900 mg of the drug was found to reduce hot flashes in women with breast cancer; however, their QOL of has not been studied. Abstract Purpose: Hot flashes are a common and debilitating symptom among survivors of breast cancer. This study aimed at evaluating the effects of electroacupuncture (EA) versus gabapentin (GP) for hot flashes among survivors of breast cancer, with a specific focus on the placebo and nocebo effects. Patients treated with gabapentin had a reduction in hot flush events and hot flush severity than those treated with placebo. Both menopausal women and patients with breast cancer benefitted from gabapentin treatment. No difference in reduction of hot flush severity was found between gabapentin and antidepressants. Breast cancer survivors prefer venlafaxine over gabapentin for treating hot flashes. Introduction Hot flashes are highly prevalent and persistent among breast cancer survivors [1]. Hot flashes are symptoms of estrogen deprivation that are exacerbated by anti-estrogen therapy used for breast cancer treatment [2, 3]. Furthermore, for pre-menopausal breast cancer patients, chemotherapy abruptly disrupts or permanently ceases ovarian function, leading to the onset of debilitating Most women receiving systemic therapy for breast cancer experience hot flashes. We undertook a randomised, double-blind, placebo-controlled, multi-institutional trial to assess the efficacy of gabapentin in controlling hot flashes in women with breast cancer. Selective serotonin reuptake inhibitors (SSRIs [fluoxetine, sertraline, paroxetine]) and the selective norepinephrine reuptake inhibitor (SNRI) venlafaxine, as well as clonidine and gabapentin, reduce hot flashes by about 25% (approximately one per day) in women with and without a history of breast cancer. The study led by Kishan J. Pandya, MD, found that gabapentin is effective in the control of hot flashes at a dose of 900 mg/day, but not the lower dose of 300 mg/day. “This drug should be considered for treatment of hot flashes in women with breast cancer,” he said. PURPOSE: Hot flashes are a common and troublesome side efect of surgery or endocrine therapy. They may lead to physical and psychological distress and negatively afect quality of life. This clinical practice guideline presents evidence-based recommendations for pharmacologic, behavioral, and natural health product interventions for treatment-related hot flashes in patients with breast or
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |