Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
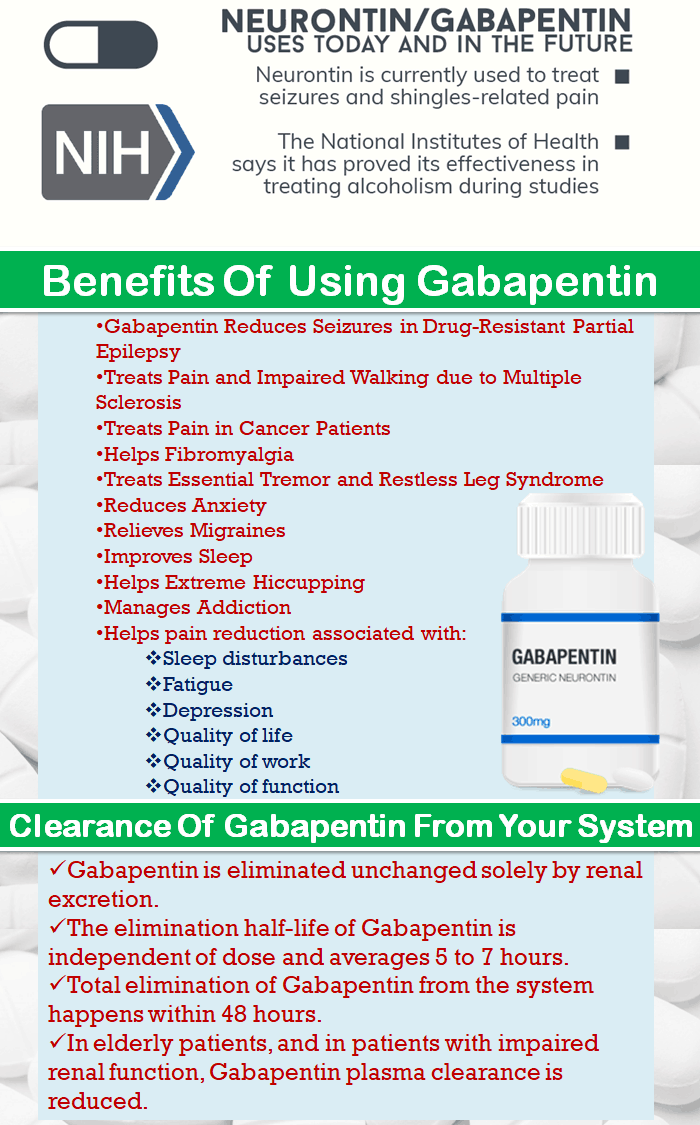
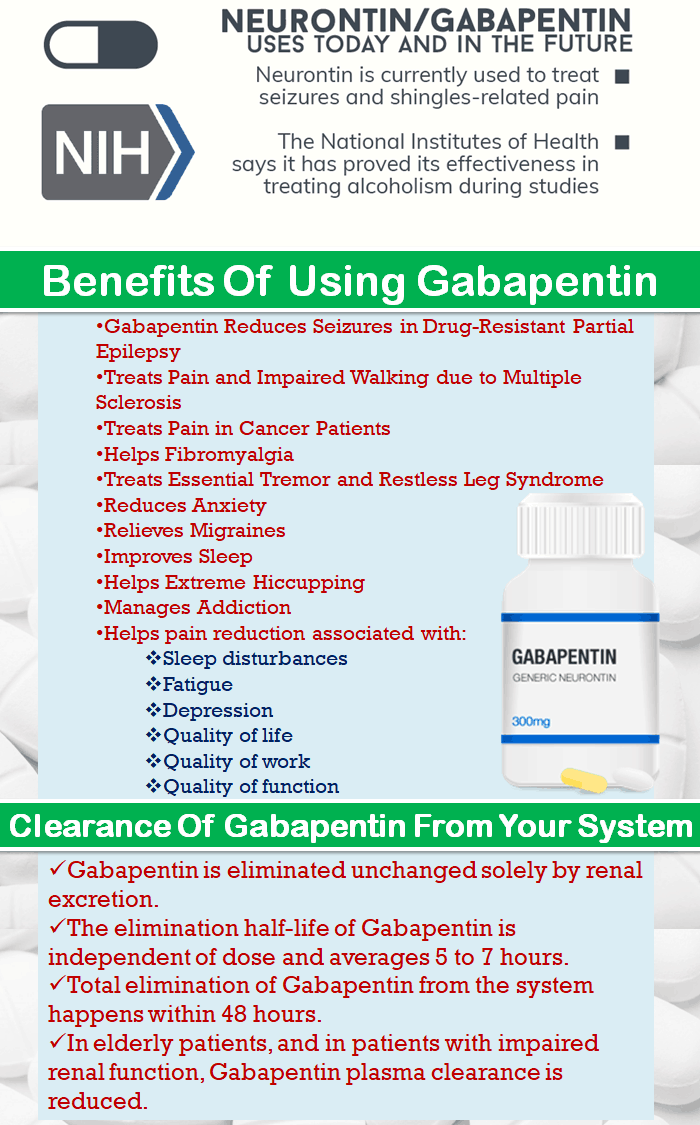
Pharmacokinetics and renal handling Challenges to achieving therapeutic concentrations necessary to achieve efficacy require consideration of the pharmacokinetic properties of both gabapentin and pregabalin. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Gabapentinoids are opioid substitutes whose elimination by the kidneys is reduced as kidney function declines. To inform their safe prescribing in older adults with chronic kidney disease (CKD), we examined the 30-day risk of serious adverse events according to the prescribed starting dose. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Background: Gabapentin and pregabalin are well-tolerated medications primarily cleared by the kidney. Patients receiving higher gabapentinoid doses with decreased kidney function may be at an increased risk of adverse effects (AEs), but limited Keywords: renal dose adjustment, gabapentin neuro, action myoclonus-renal failure syndrome, severe diabetic neuropathy, painful neuropathy, ckd management, pain management in ckd patients, ckd, drug-induced myoclonus, pregabalin and gabapentin treatment for peripheral neuropathy Introduction Introduction Renal dose adjustments for gabapentin and pregabalin are ubiquitously evident in the medical literature. All manufacturers for these branded and generic dosage forms list dosing recommendations relative to creatinine clearance (CrCl) for both medications (Table 1).1,2 However, the basis of these recommendations has not been well articulated. Gabapentinoids, including gabapentin and pregabalin, are frequently prescribed as opioid alternatives. Given that gabapentinoids are eliminated from the body by the kidney, we sought to determine the risk of serious adverse events in patients with chronic kidney disease who started a gabapentinoid at a higher versus a lower dose. Gabapentin and pregabalin are often used in patients with CKD primarily to treat neuropathic pain and restless leg syndrome and given the high prevalence of diabetes in this population, the proportion who receive these drugs is very high. In patients with normal renal function, the maximum dose of gabapentin is 3600mg daily in divided doses. However, gabapentin is renally cleared and so the Gabapentin can be used by kidney disease patients, but dosage adjustments are critical. Learn how to safely use gabapentin with kidney issues and discover alternative medications. Gabapentinoids, including gabapentin and pregabalin, are frequently prescribed as opioid alternatives. Given that gabapentinoids are eliminated from the body by the kidney, we sought to determine the risk of serious adverse events in patients with chronic kidney disease who started a gabapentinoid at a higher versus a lower dose. INTRODUCTION Pain is one of the most common and distressing symptoms among patients with chronic kidney disease (CKD) [1]. The prevalence of pain has been associated with substantially lower health-related quality of life and greater psychosocial distress, insomnia, and depressive symptoms [2-9]. Among hemodialysis patients, severe pain is also independently associated with shortened or missed Studies have shown that gabapentin toxicity can occur in patients with chronic kidney disease, particularly in those with advanced age and multiple comorbidities 4, 5. Dose Adjustment and Renal Function Dose adjustment of gabapentin is crucial in patients with decreased renal function to prevent toxicity 4, 5. Gabapentin, a medication primarily used to treat nerve pain and seizures, has gained attention for its effectiveness and relatively mild side effects compared to other analgesics. However, concerns about its impact on kidney health have surfaced, prompting patients and healthcare providers to question: Can Gabapentin Cause Kidney Problems? Understanding this relationship is vital for those Gabapentin is widely used in the management of pain. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. Abstract Background: Gabapentinoids (GPs) are frequently prescribed in individuals with chronic kidney disease (CKD); however, their exclusive renal elimination warrants dose adjustments to decrease risk of toxicity. This study evaluated GP prescribing patterns and whether excessive dosing was associated with increased incidence of gabapentinoid-related adverse events (GRAEs). Gabapentin is a prescription drug for seizures and nerve pain. It usually doesn’t harm the liver or kidneys, but it can cause a rare allergic reaction called DRESS syndrome. Learn about gabapentin dosing, side effects, and interactions. Structure of GABA: gabapentin and pregabalin. 10 Pharmacokinetics The actions of gabapentinoids are mainly at an intracellular site and require active uptake. They undergo facilitated transport across cell membranes through system l -amino acid transporters (LAT) as both drugs are structurally similar to the amino acid leucine. The effects of chronic gabapentin are blocked by an inhibitor of Neurontin - Gabapentin Renal Dosing protocol for Adults, maintenance gabapentin dosing and additional dosing for adults undergoing dialysis Gabapentin is actually toxic to the kidneys. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its well recieved pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |